Back

Poster Session B - Monday Morning
Category: Endoscopy Video Forum
B0192 - A Palliative Approach: Stenting a Malignant Duodenocolonic Fistula in a Patient With Two Primary Malignancies
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- YH
Yassmin Hegazy, MD
University of Alabama at Birmingham
Birmingham, AL
Presenting Author(s)
Yassmin Hegazy, MD, Ramzi Mulki, MD, Usman Barlass, MD, Ali M. Ahmed, MD, Kondal R. Kyanam Kabir Baig, MD, Shajan Peter, MD
University of Alabama at Birmingham, Birmingham, AL
Introduction: Duodenocolonic fistulas can be complications of malignancy with management being challenging for non-surgical patients. Our case highlights a palliative approach by duodenal stenting in a malignant duodenocolonic fistula.
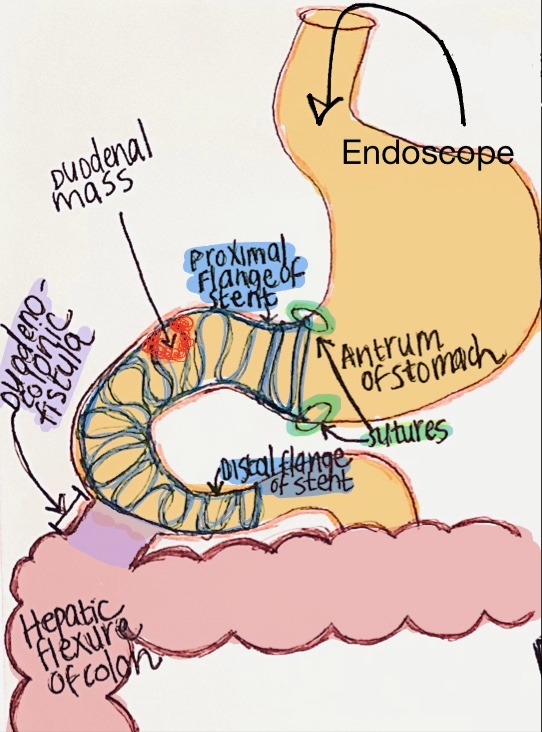
Case Description/Methods: A 73-year-old male with a history of Diabetes Mellitus presents with a one-week history of hematochezia with associated epigastric pain. On admission, his vitals were stable and he had bright red blood on rectal exam. Labs were notable for a calcium 7 mg/dL, magnesium 1.2 mg/dL and hemoglobin 9.8 gm/dL. Computed tomography (CT) imaging revealed a pulmonary mass and a duodenocolonic fistula. The patient underwent an upper GI endoscopy with findings revealing a 10 millimeter (mm) fistula in the first and second portion of the duodenum with opening into the right side of the colon and an infiltrative mass past the duodenal bulb with biopsy positive for invasive adenocarcinoma. A 20mm x 120mm covered metal luminal stent was placed under fluoroscopy with the proximal flange in the antrum of the stomach and distal flange in the second part of the duodenum, bridging the fistula (Figure 1). The stent was anchored proximally by the endoscopic placement of two interrupted 2.0 polypropylene sutures to prevent distal migration. Fluoroscopy revealed no contrast extravasation with good flow into the proximal jejunum. Interval imaging three weeks post-procedure revealed a second primary lung malignancy. The patient was seen in clinic one month following the procedure with improved abdominal pain and tolerating a full-liquid diet.
Discussion: This case highlights an endoscopic approach to stenting a duodenocolonic fistula. While the treatment for malignant dudoenocolonic fistula can include surgery such as hemicolectomy, parental nutrition is usually required with the risk of post-operative complications. Alternative endoscopic approaches including using through the scope or over the scope clips for enteral fistula closure has a higher likelihood of dislodging and failure given their smaller size relative to the fistula. Other techniques including endoscopic suturing would not be ideal given the friability associated with the tumor causing the sutures to fail and dehisce. A covered duodenal stent placed across the fistula allowed for a less invasive method to relieve debilitating vomiting and abdominal pain. Our case demonstrates an endoscopic palliative method in providing symptom relief and insuring enteral nutrition in patients with a limited life expectancy.
Disclosures:
Yassmin Hegazy, MD, Ramzi Mulki, MD, Usman Barlass, MD, Ali M. Ahmed, MD, Kondal R. Kyanam Kabir Baig, MD, Shajan Peter, MD. B0192 - A Palliative Approach: Stenting a Malignant Duodenocolonic Fistula in a Patient With Two Primary Malignancies, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Alabama at Birmingham, Birmingham, AL
Introduction: Duodenocolonic fistulas can be complications of malignancy with management being challenging for non-surgical patients. Our case highlights a palliative approach by duodenal stenting in a malignant duodenocolonic fistula.
Case Description/Methods: A 73-year-old male with a history of Diabetes Mellitus presents with a one-week history of hematochezia with associated epigastric pain. On admission, his vitals were stable and he had bright red blood on rectal exam. Labs were notable for a calcium 7 mg/dL, magnesium 1.2 mg/dL and hemoglobin 9.8 gm/dL. Computed tomography (CT) imaging revealed a pulmonary mass and a duodenocolonic fistula. The patient underwent an upper GI endoscopy with findings revealing a 10 millimeter (mm) fistula in the first and second portion of the duodenum with opening into the right side of the colon and an infiltrative mass past the duodenal bulb with biopsy positive for invasive adenocarcinoma. A 20mm x 120mm covered metal luminal stent was placed under fluoroscopy with the proximal flange in the antrum of the stomach and distal flange in the second part of the duodenum, bridging the fistula (Figure 1). The stent was anchored proximally by the endoscopic placement of two interrupted 2.0 polypropylene sutures to prevent distal migration. Fluoroscopy revealed no contrast extravasation with good flow into the proximal jejunum. Interval imaging three weeks post-procedure revealed a second primary lung malignancy. The patient was seen in clinic one month following the procedure with improved abdominal pain and tolerating a full-liquid diet.
Discussion: This case highlights an endoscopic approach to stenting a duodenocolonic fistula. While the treatment for malignant dudoenocolonic fistula can include surgery such as hemicolectomy, parental nutrition is usually required with the risk of post-operative complications. Alternative endoscopic approaches including using through the scope or over the scope clips for enteral fistula closure has a higher likelihood of dislodging and failure given their smaller size relative to the fistula. Other techniques including endoscopic suturing would not be ideal given the friability associated with the tumor causing the sutures to fail and dehisce. A covered duodenal stent placed across the fistula allowed for a less invasive method to relieve debilitating vomiting and abdominal pain. Our case demonstrates an endoscopic palliative method in providing symptom relief and insuring enteral nutrition in patients with a limited life expectancy.
Figure: Figure 1: Anatomy of stent placement position with proximal flange of the stent placed in the antrum of the stomach and distal flange in the second part of the duodenum.
Disclosures:
Yassmin Hegazy indicated no relevant financial relationships.
Ramzi Mulki indicated no relevant financial relationships.
Usman Barlass indicated no relevant financial relationships.
Ali Ahmed indicated no relevant financial relationships.
Kondal Kyanam Kabir Baig: Ambu – Consultant. Ambu – Grant/Research Support. Olympus – Grant/Research Support.
Shajan Peter indicated no relevant financial relationships.
Yassmin Hegazy, MD, Ramzi Mulki, MD, Usman Barlass, MD, Ali M. Ahmed, MD, Kondal R. Kyanam Kabir Baig, MD, Shajan Peter, MD. B0192 - A Palliative Approach: Stenting a Malignant Duodenocolonic Fistula in a Patient With Two Primary Malignancies, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
