Back

Poster Session B - Monday Morning
Category: Endoscopy Video Forum
B0193 - Dysphagia From an Ischemic Colonic Segment in a Patient With Colon Interposition
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- YH
Yassmin Hegazy, MD
University of Alabama at Birmingham
Birmingham, AL
Presenting Author(s)
Yassmin Hegazy, MD1, Usman Barlass, MD1, Douglas Morgan, MD, MPH1, Dane Johnson, MD1, Pooja Bhavsar, BS2, Kondal R. Kyanam Kabir Baig, MD1
1University of Alabama at Birmingham, Birmingham, AL; 2Byramjee Jeejeebhoy Medical College, Ahmedabad, Gujarat, India
Introduction: Colon interposition of the esophagus in adults may lead to future complications including chronic ischemia, stricture formation, and adenocarcinoma.
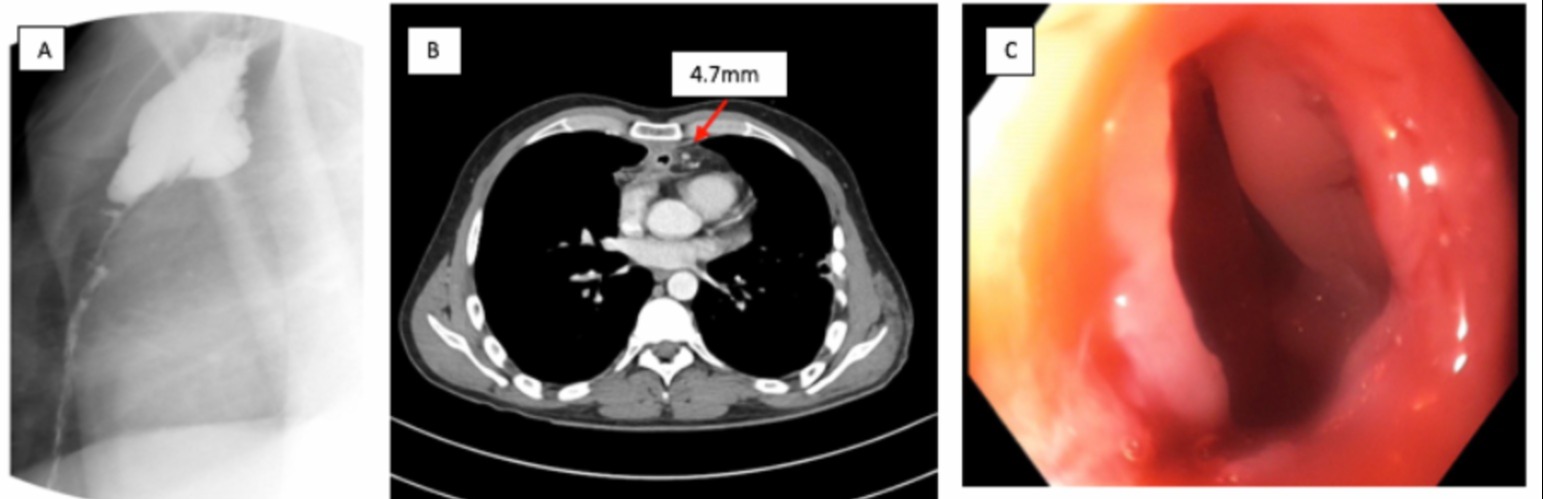
Case Description/Methods: A 39-year-old male immigrant presented with progressive dysphagia, in the setting of a remote history of emergent colon interposition following gunshot wounds of the esophagus. In the prior 6 months, he developed dysphagia with solids and then liquids, with associated weight loss and regurgitation. On admission, he had stable vitals with an unremarkable physical exam and labs. Esophagram revealed a severe high-grade, upper-mid esophageal stricture with proximal dilation (Figure 1A). Computed Tomography (CT) imaging showed an esophageal conduit in the anterior mediastinum with proximal conduit distension and distal conduit narrowing (Figure 1B).
Esophagoduodenoscopy (EGD) revealed a stricture (6 mm) at the esophago-colonic anastomosis, 19 cm from the incisors (Figure 1C). This was traversed with an ultra-thin endoscope which also revealed a severe stenosis distally in the colon segment with a partially obstructing inflammatory polyp. The proximal stricture was dilated in a staged fashion to advance the upper endoscope to the colonic stenosis. A wire was advanced and the stenosis length was estimated to be 11 cm under fluoroscopy. This was successfully stented with 20 mm x 12 cm covered metal stent.
The stent was removed one month following the procedure with initial improvement in dysphagia and a normalized diet. However, the patient had re-occurring symptoms and a repeat EGD with dilation and stenting was performed one week later. The multidisciplinary team recommended definitive treatment for the chronic ischemic segment-related complications.
Discussion: Conduit ischemia with anastomotic strictures can occur in patients with a history of colonic interposition. Evaluation with double contrast studies may reveal ischemic changes including loss of haustration and stricture formation in the colon graft with dilation being an effective treatment. Chronic ischemia can be a delayed complication of the interposed colon resulting from non-necrotic vascular insufficiency leading to fibrosis, stricture formation, and dysphagia. Additionally, given the patient’s stricture and mass, there was concern for underlying malignancy, which highlights the utility of adenocarcinoma screening in this patient population.
Disclosures:
Yassmin Hegazy, MD1, Usman Barlass, MD1, Douglas Morgan, MD, MPH1, Dane Johnson, MD1, Pooja Bhavsar, BS2, Kondal R. Kyanam Kabir Baig, MD1. B0193 - Dysphagia From an Ischemic Colonic Segment in a Patient With Colon Interposition, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Alabama at Birmingham, Birmingham, AL; 2Byramjee Jeejeebhoy Medical College, Ahmedabad, Gujarat, India
Introduction: Colon interposition of the esophagus in adults may lead to future complications including chronic ischemia, stricture formation, and adenocarcinoma.
Case Description/Methods: A 39-year-old male immigrant presented with progressive dysphagia, in the setting of a remote history of emergent colon interposition following gunshot wounds of the esophagus. In the prior 6 months, he developed dysphagia with solids and then liquids, with associated weight loss and regurgitation. On admission, he had stable vitals with an unremarkable physical exam and labs. Esophagram revealed a severe high-grade, upper-mid esophageal stricture with proximal dilation (Figure 1A). Computed Tomography (CT) imaging showed an esophageal conduit in the anterior mediastinum with proximal conduit distension and distal conduit narrowing (Figure 1B).
Esophagoduodenoscopy (EGD) revealed a stricture (6 mm) at the esophago-colonic anastomosis, 19 cm from the incisors (Figure 1C). This was traversed with an ultra-thin endoscope which also revealed a severe stenosis distally in the colon segment with a partially obstructing inflammatory polyp. The proximal stricture was dilated in a staged fashion to advance the upper endoscope to the colonic stenosis. A wire was advanced and the stenosis length was estimated to be 11 cm under fluoroscopy. This was successfully stented with 20 mm x 12 cm covered metal stent.
The stent was removed one month following the procedure with initial improvement in dysphagia and a normalized diet. However, the patient had re-occurring symptoms and a repeat EGD with dilation and stenting was performed one week later. The multidisciplinary team recommended definitive treatment for the chronic ischemic segment-related complications.
Discussion: Conduit ischemia with anastomotic strictures can occur in patients with a history of colonic interposition. Evaluation with double contrast studies may reveal ischemic changes including loss of haustration and stricture formation in the colon graft with dilation being an effective treatment. Chronic ischemia can be a delayed complication of the interposed colon resulting from non-necrotic vascular insufficiency leading to fibrosis, stricture formation, and dysphagia. Additionally, given the patient’s stricture and mass, there was concern for underlying malignancy, which highlights the utility of adenocarcinoma screening in this patient population.
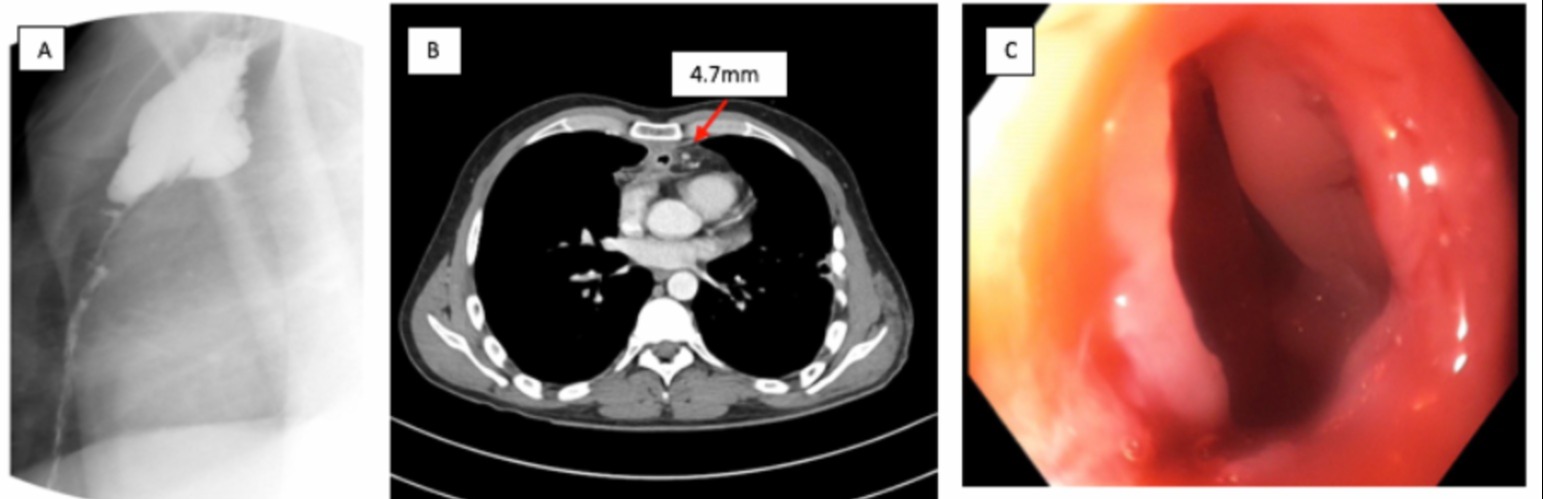
Figure: 1A: Esophagram showing severe high-grade stricture at the junction of the cranial one third and distal two thirds of the esophagus. 1B: CT chest showing conduit extending along anterior mediastinum and deep into the sternum with anastomosis in upper neck and abrupt caliber change in mid esophageal conduit at level of right main pulmonary artery with associated wall thickening, fat stranding, and small adjacent lymph nodes measuring up to 5mm (red arrow). 1C: Esophago-colonic anastomosis found in the middle/lower third of the esophagus at 29cm from incisors.
Disclosures:
Yassmin Hegazy indicated no relevant financial relationships.
Usman Barlass indicated no relevant financial relationships.
Douglas Morgan: Cancer Prevention Pharmaceuticals – NCI funded study, company donated study medications.. CDx Diagnostics – Investigator initiated study, company donated disposables.. Freenome – Grant/Research Support. Thorne Research – NCI funded study, company donated study medications..
Dane Johnson indicated no relevant financial relationships.
Pooja Bhavsar indicated no relevant financial relationships.
Kondal Kyanam Kabir Baig: Ambu – Consultant. Ambu – Grant/Research Support. Olympus – Grant/Research Support.
Yassmin Hegazy, MD1, Usman Barlass, MD1, Douglas Morgan, MD, MPH1, Dane Johnson, MD1, Pooja Bhavsar, BS2, Kondal R. Kyanam Kabir Baig, MD1. B0193 - Dysphagia From an Ischemic Colonic Segment in a Patient With Colon Interposition, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
