Back

Poster Session B - Monday Morning
Category: Endoscopy Video Forum
B0195 - Endoscopic Eversion and Stent-Assisted Strangulation for the Management of an Intraductal Papillary Neoplasm of the Bile Duct: A Minimally Invasive Technique for Non-Surgical Candidates
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Debdeep Banerjee, MD
University of Alabama at Birmingham School of Medicine
Birmingham, AL
Presenting Author(s)
Debdeep Banerjee, MD1, Usman Barlass, MD2, Ramzi Mulki, MD2, Rachel Mitchell, CRNP3, Ali M. Ahmed, MD2, Shajan Peter, MD2, Kondal R. Kyanam Kabir Baig, MD2, Sergio A. Sánchez-Luna, MD3
1University of Alabama at Birmingham School of Medicine, Birmingham, AL; 2University of Alabama at Birmingham, Birmingham, AL; 3University of Alabama Birmingham, Birmingham, AL
Introduction: Intraductal papillary neoplasms of the bile duct (IPNB) are uncommon lesions that may accompany risk for malignancy. Management is often surgical and may be associated with significant postoperative morbidity and mortality.
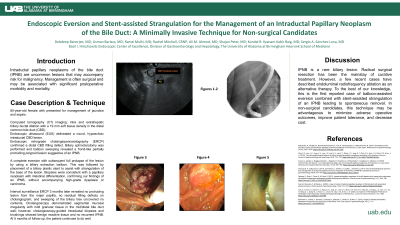
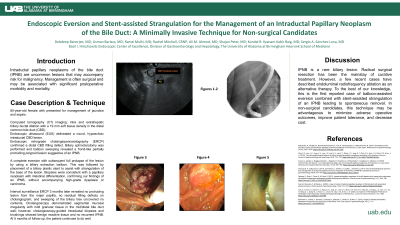
Case Description/Methods: An 80-year-old female with a history of hepatocellular carcinoma (HCC) presented for management of jaundice and sepsis after microwave ablation of HCC. Computed tomography (CT) imaging demonstrated intra and extrahepatic biliary ductal dilation with a 19 mm soft tissue density in the distal common bile duct (CBD). Index labs depicted leukocytosis, hyperbilirubinemia, and elevated lactate. Endoscopic ultrasound (EUS) delineated a round, hypoechoic intraductal CBD lesion. The pancreas and ampulla were normal. Endoscopic retrograde cholangiopancreatography (ERCP) confirmed a distal CBD filling defect. Biliary sphincterotomy was performed and balloon sweeping revealed a frond-like partially protruding polypoid lesion suggestive of an IPNB. Due to non-surgical candidacy, we decided to perform a complete eversion with subsequent full prolapse of the lesion by using a biliary extraction balloon. This was followed by the placement of a biliary plastic stent to assist with strangulation of the base of the lesion. Biopsies were consistent with a papillary neoplasm with intestinal differentiation, confirming our findings of an IPNB, without accompanying high-grade dysplasia or carcinoma. Interval surveillance ERCP 3 months later revealed no protruding lesion from the major papilla, no residual filling defects on cholangiogram, and sweeping of the biliary tree uncovered no contents. Cholangioscopy demonstrated segmental mucosal irregularity with mild granular tissue in the mid/distal bile duct wall; however, cholangioscopy-guided intraductal biopsies and brushings showed benign reactive tissue and no recurrent IPNB. At 5 months of follow-up, the patient continues to do well.
Discussion: IPNB is a rare biliary lesion. Radical surgical resection has been the mainstay of curative treatment. However, a few recent cases have described endoluminal radiofrequency ablation as an alternative therapy. To the best of our knowledge, this is the first reported case of balloon-assisted eversion combined with stent-assisted strangulation of an IPNB leading to spontaneous removal. In non-surgical candidates, this technique may be advantageous to minimize adverse operative outcomes, improve patient tolerance, and decrease cost.
Disclosures:
Debdeep Banerjee, MD1, Usman Barlass, MD2, Ramzi Mulki, MD2, Rachel Mitchell, CRNP3, Ali M. Ahmed, MD2, Shajan Peter, MD2, Kondal R. Kyanam Kabir Baig, MD2, Sergio A. Sánchez-Luna, MD3. B0195 - Endoscopic Eversion and Stent-Assisted Strangulation for the Management of an Intraductal Papillary Neoplasm of the Bile Duct: A Minimally Invasive Technique for Non-Surgical Candidates, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Alabama at Birmingham School of Medicine, Birmingham, AL; 2University of Alabama at Birmingham, Birmingham, AL; 3University of Alabama Birmingham, Birmingham, AL
Introduction: Intraductal papillary neoplasms of the bile duct (IPNB) are uncommon lesions that may accompany risk for malignancy. Management is often surgical and may be associated with significant postoperative morbidity and mortality.
Case Description/Methods: An 80-year-old female with a history of hepatocellular carcinoma (HCC) presented for management of jaundice and sepsis after microwave ablation of HCC. Computed tomography (CT) imaging demonstrated intra and extrahepatic biliary ductal dilation with a 19 mm soft tissue density in the distal common bile duct (CBD). Index labs depicted leukocytosis, hyperbilirubinemia, and elevated lactate. Endoscopic ultrasound (EUS) delineated a round, hypoechoic intraductal CBD lesion. The pancreas and ampulla were normal. Endoscopic retrograde cholangiopancreatography (ERCP) confirmed a distal CBD filling defect. Biliary sphincterotomy was performed and balloon sweeping revealed a frond-like partially protruding polypoid lesion suggestive of an IPNB. Due to non-surgical candidacy, we decided to perform a complete eversion with subsequent full prolapse of the lesion by using a biliary extraction balloon. This was followed by the placement of a biliary plastic stent to assist with strangulation of the base of the lesion. Biopsies were consistent with a papillary neoplasm with intestinal differentiation, confirming our findings of an IPNB, without accompanying high-grade dysplasia or carcinoma. Interval surveillance ERCP 3 months later revealed no protruding lesion from the major papilla, no residual filling defects on cholangiogram, and sweeping of the biliary tree uncovered no contents. Cholangioscopy demonstrated segmental mucosal irregularity with mild granular tissue in the mid/distal bile duct wall; however, cholangioscopy-guided intraductal biopsies and brushings showed benign reactive tissue and no recurrent IPNB. At 5 months of follow-up, the patient continues to do well.
Discussion: IPNB is a rare biliary lesion. Radical surgical resection has been the mainstay of curative treatment. However, a few recent cases have described endoluminal radiofrequency ablation as an alternative therapy. To the best of our knowledge, this is the first reported case of balloon-assisted eversion combined with stent-assisted strangulation of an IPNB leading to spontaneous removal. In non-surgical candidates, this technique may be advantageous to minimize adverse operative outcomes, improve patient tolerance, and decrease cost.
Disclosures:
Debdeep Banerjee indicated no relevant financial relationships.
Usman Barlass indicated no relevant financial relationships.
Ramzi Mulki indicated no relevant financial relationships.
Rachel Mitchell indicated no relevant financial relationships.
Ali Ahmed indicated no relevant financial relationships.
Shajan Peter indicated no relevant financial relationships.
Kondal Kyanam Kabir Baig: Ambu – Consultant. Ambu – Grant/Research Support. Olympus – Grant/Research Support.
Sergio Sánchez-Luna indicated no relevant financial relationships.
Debdeep Banerjee, MD1, Usman Barlass, MD2, Ramzi Mulki, MD2, Rachel Mitchell, CRNP3, Ali M. Ahmed, MD2, Shajan Peter, MD2, Kondal R. Kyanam Kabir Baig, MD2, Sergio A. Sánchez-Luna, MD3. B0195 - Endoscopic Eversion and Stent-Assisted Strangulation for the Management of an Intraductal Papillary Neoplasm of the Bile Duct: A Minimally Invasive Technique for Non-Surgical Candidates, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

