Back

Poster Session A - Sunday Afternoon
Category: Liver
A0550 - Treatment of Invasive Liver Abscess Syndrome With Limited Percutaneous Drainage and Antibiotics
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Levon Tantoushian, DO
Valley Hospital Medical Center
Las Vegas, NV
Presenting Author(s)
Levon Tantoushian, DO, Kory Cummings, DO, Thomas Ilustrisimo, DO, Mark McKenzie, MD, Paul Kalekas, DO
Valley Hospital Medical Center, Las Vegas, NV
Introduction: Klebsiella pneumoniae primary liver abscess (KLA) is characterized by bacteremia, liver abscesses, and metastatic infections. It is prevalent in Asian countries but has been rarely documented in the U.S. with approximately 20 documented cases as of 2007 [1]. KLA often originates as a single liver mass, but complications include multiple liver lesions, endophthalmitis, meningitis, or distant abscesses. First line therapy involves abscess drainage. We present a case of KLA in a patient with multiple liver abscesses which were unable to be entirely drained due to location and quantity. This case highlights the ability to treat KLA with a combination of abscess drainage and systemic antibiotics to remove inaccessible abscesses, preventing complications, and surgical resection.
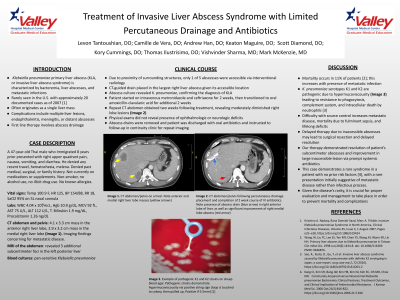
Case Description/Methods: A 47-year-old Thai male who immigrated 8 years prior presented with right upper quadrant pain, nausea, vomiting, and diarrhea. He was febrile, tachcyardic and found to have a mild transaminitis and elevated procalcitonin. CT of the abdomen and pelvis showed a 4.1 x 3.3 cm mass in the anterior right liver lobe and a 2.9 x 3.2 cm mass in the medial right liver lobe. MRI of the abdomen revealed 3 additional subcentimeter foci in the left posterior liver. Blood cultures grew pansensitive Klebsiella pneumoniae. He underwent CT guided drain placement in the largest right liver abscess due to location and size of remaining liver masses. Abscess culture confirmed diagnosis of KLA. Intravenous antibiotics with metronidazole and ceftriaxone were completed for 2 weeks, followed by transition to oral amoxicillin-clavulanic acid for an additional 2 weeks. Repeat CT abdomen was obtained one week following treatment, revealing moderately diminished right lobe lesions. Patient’s symptoms improved and transaminitis resolved. Abscess drains were removed, patient was discharged with oral antibiotics and instructed to follow-up in continuity clinic for repeat imaging.
Discussion: Invasive liver abscess syndrome is a phenomenon which typically affects the Southeast Asian population, but is extremely rare within the United States. Complications and mortality arise due to metastatic disease, fulminant sepsis, and lifelong deficits. Our case presented a patient with no risk factors who developed multiple liver abscesses, of which only 1 was accessible via percutaneous drainage. With our therapy, the abscesses were treated appropriately, avoiding further invasive source control and metastatic complications.
Disclosures:
Levon Tantoushian, DO, Kory Cummings, DO, Thomas Ilustrisimo, DO, Mark McKenzie, MD, Paul Kalekas, DO. A0550 - Treatment of Invasive Liver Abscess Syndrome With Limited Percutaneous Drainage and Antibiotics, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Valley Hospital Medical Center, Las Vegas, NV
Introduction: Klebsiella pneumoniae primary liver abscess (KLA) is characterized by bacteremia, liver abscesses, and metastatic infections. It is prevalent in Asian countries but has been rarely documented in the U.S. with approximately 20 documented cases as of 2007 [1]. KLA often originates as a single liver mass, but complications include multiple liver lesions, endophthalmitis, meningitis, or distant abscesses. First line therapy involves abscess drainage. We present a case of KLA in a patient with multiple liver abscesses which were unable to be entirely drained due to location and quantity. This case highlights the ability to treat KLA with a combination of abscess drainage and systemic antibiotics to remove inaccessible abscesses, preventing complications, and surgical resection.
Case Description/Methods: A 47-year-old Thai male who immigrated 8 years prior presented with right upper quadrant pain, nausea, vomiting, and diarrhea. He was febrile, tachcyardic and found to have a mild transaminitis and elevated procalcitonin. CT of the abdomen and pelvis showed a 4.1 x 3.3 cm mass in the anterior right liver lobe and a 2.9 x 3.2 cm mass in the medial right liver lobe. MRI of the abdomen revealed 3 additional subcentimeter foci in the left posterior liver. Blood cultures grew pansensitive Klebsiella pneumoniae. He underwent CT guided drain placement in the largest right liver abscess due to location and size of remaining liver masses. Abscess culture confirmed diagnosis of KLA. Intravenous antibiotics with metronidazole and ceftriaxone were completed for 2 weeks, followed by transition to oral amoxicillin-clavulanic acid for an additional 2 weeks. Repeat CT abdomen was obtained one week following treatment, revealing moderately diminished right lobe lesions. Patient’s symptoms improved and transaminitis resolved. Abscess drains were removed, patient was discharged with oral antibiotics and instructed to follow-up in continuity clinic for repeat imaging.
Discussion: Invasive liver abscess syndrome is a phenomenon which typically affects the Southeast Asian population, but is extremely rare within the United States. Complications and mortality arise due to metastatic disease, fulminant sepsis, and lifelong deficits. Our case presented a patient with no risk factors who developed multiple liver abscesses, of which only 1 was accessible via percutaneous drainage. With our therapy, the abscesses were treated appropriately, avoiding further invasive source control and metastatic complications.
Disclosures:
Levon Tantoushian indicated no relevant financial relationships.
Kory Cummings indicated no relevant financial relationships.
Thomas Ilustrisimo indicated no relevant financial relationships.
Mark McKenzie indicated no relevant financial relationships.
Paul Kalekas indicated no relevant financial relationships.
Levon Tantoushian, DO, Kory Cummings, DO, Thomas Ilustrisimo, DO, Mark McKenzie, MD, Paul Kalekas, DO. A0550 - Treatment of Invasive Liver Abscess Syndrome With Limited Percutaneous Drainage and Antibiotics, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
