Back

Poster Session A - Sunday Afternoon
Category: Colon
A0106 - A Rare Case of Metastatic Primary Rectal Melanoma in a Geriatric Patient
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Onyinye Ugonabo, MD
Marshall University Joan C. Edwards School of Medicine
HUNTINGTON, WV
Presenting Author(s)
Onyinye Ugonabo, MD1, Mujtaba Mohamed, MD1, Ebubechukwu Ezeh, MD2, Pramod Pantangi, MD1, Shima Ghavimi, MD3
1Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 2Marshall University Hospital School of Medicine, Huntington, WV; 3Marshall University, Ona, WV
Introduction: Primary rectal melanoma (PRM) is a very rare and aggressive malignancy. It constitutes about 0.5‑4% of all anorectal malignancies and less than 1% of all melanomas (1). It is more common in women and usually present in the fifth or sixth decade of life (1). The most common presenting symptom is rectal bleeding. Prognosis is poor with a median survival of 24 months and 5-year survival of 10%.
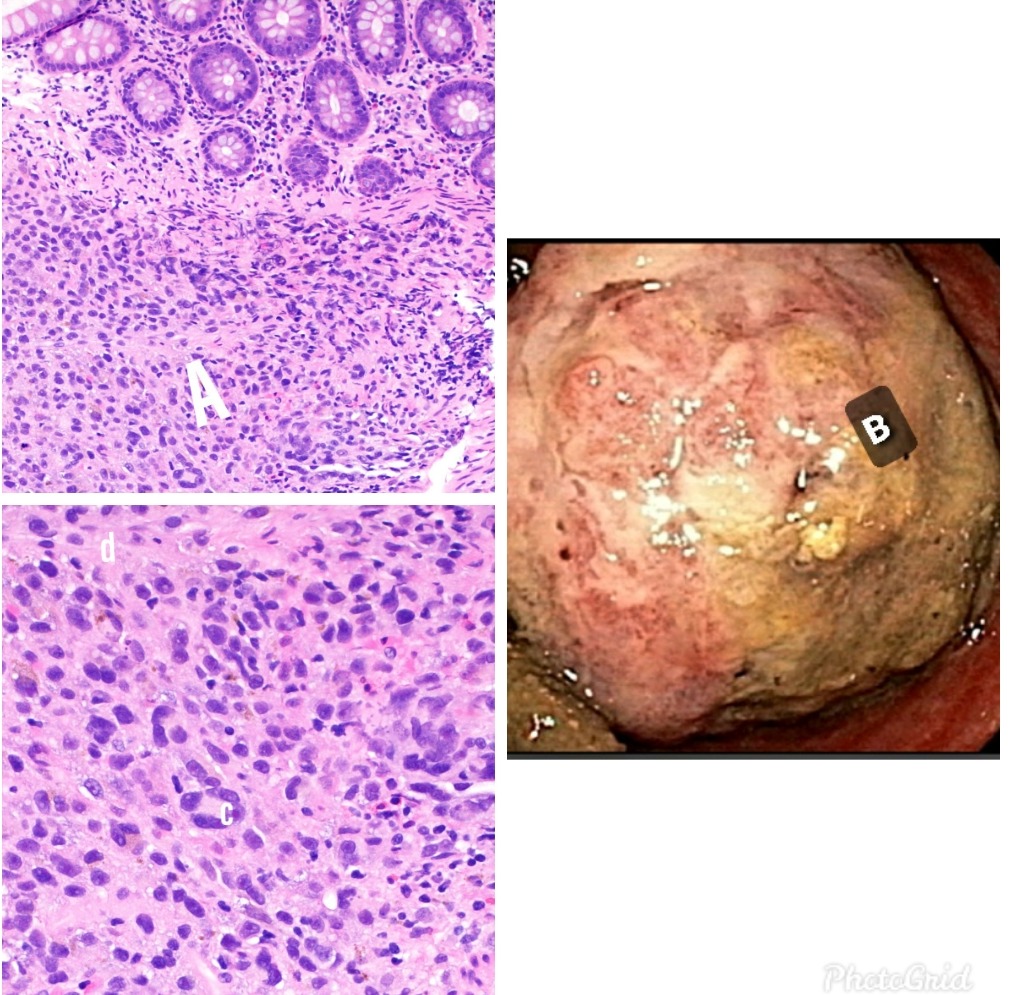
Case Description/Methods: A 72-year-old male, presented with bleeding per rectum, anal mass, and diarrhea for 11 months associated with anal pruritus. Significant examination findings include a soft, painful, friable mass protruding through the anus. The skin exam was negative for any abnormal skin pigmentation. Laboratory data was only remarkable for hemoglobin of 9.8gm/dl. CT abdomen and pelvis showed numerous hepatic lesions, with the largest measuring 2.4cm, a large soft tissue at the anorectal junction with bilateral inguinal lymphadenopathy. Colonoscopy showed a friable mass at the anus, measuring about 3cm, fig B. Biopsy showed pigment-containing atypical pleomorphic cells positive for S100 and Sox 10 confirming the diagnosis of malignant rectal melanoma, Figs Acd. The patient opted for hospice care.
Discussion: PRM is defined as melanoma arising from melanocytes in the rectal mucosa, more than 4 cm from the anal verge. Lymphatic metastasis to the inguinal or inferior mesenteric lymph nodes is common. Biopsy through colonoscopy or proctoscopy is the gold standard to establish the diagnosis. CT and Magnetic resonance imaging aid characterization, extent of the tumor and tumor staging. Useful markers commonly used include S100 protein, HMB 45, melanin A, and Sox 10. Multiple studies support that an abdominoperineal resection is the treatment of choice. This is based on the hypothesis that the disease spreads proximally via the submucosa to the mesenteric lymph nodes. Surgical resection with free margins is the goal of surgical treatment. New therapies are being studied, including immunotherapy, which can improve the dismal prognosis of this rare disease. The rarity of this disease and the limited number of patients presenting with the early disease have prevented definitive trials examining the optimal treatment for anal melanoma.
Reference
1. Kohli S, Narang S, Singhal A, Kumar V, Kaur O, Chandoke R. Malignant melanoma of the rectum. J Clin Imaging Sci. 2014;4:4. Published 2014 Jan 30. doi:10.4103/2156-7514.126031
Disclosures:
Onyinye Ugonabo, MD1, Mujtaba Mohamed, MD1, Ebubechukwu Ezeh, MD2, Pramod Pantangi, MD1, Shima Ghavimi, MD3. A0106 - A Rare Case of Metastatic Primary Rectal Melanoma in a Geriatric Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 2Marshall University Hospital School of Medicine, Huntington, WV; 3Marshall University, Ona, WV
Introduction: Primary rectal melanoma (PRM) is a very rare and aggressive malignancy. It constitutes about 0.5‑4% of all anorectal malignancies and less than 1% of all melanomas (1). It is more common in women and usually present in the fifth or sixth decade of life (1). The most common presenting symptom is rectal bleeding. Prognosis is poor with a median survival of 24 months and 5-year survival of 10%.
Case Description/Methods: A 72-year-old male, presented with bleeding per rectum, anal mass, and diarrhea for 11 months associated with anal pruritus. Significant examination findings include a soft, painful, friable mass protruding through the anus. The skin exam was negative for any abnormal skin pigmentation. Laboratory data was only remarkable for hemoglobin of 9.8gm/dl. CT abdomen and pelvis showed numerous hepatic lesions, with the largest measuring 2.4cm, a large soft tissue at the anorectal junction with bilateral inguinal lymphadenopathy. Colonoscopy showed a friable mass at the anus, measuring about 3cm, fig B. Biopsy showed pigment-containing atypical pleomorphic cells positive for S100 and Sox 10 confirming the diagnosis of malignant rectal melanoma, Figs Acd. The patient opted for hospice care.
Discussion: PRM is defined as melanoma arising from melanocytes in the rectal mucosa, more than 4 cm from the anal verge. Lymphatic metastasis to the inguinal or inferior mesenteric lymph nodes is common. Biopsy through colonoscopy or proctoscopy is the gold standard to establish the diagnosis. CT and Magnetic resonance imaging aid characterization, extent of the tumor and tumor staging. Useful markers commonly used include S100 protein, HMB 45, melanin A, and Sox 10. Multiple studies support that an abdominoperineal resection is the treatment of choice. This is based on the hypothesis that the disease spreads proximally via the submucosa to the mesenteric lymph nodes. Surgical resection with free margins is the goal of surgical treatment. New therapies are being studied, including immunotherapy, which can improve the dismal prognosis of this rare disease. The rarity of this disease and the limited number of patients presenting with the early disease have prevented definitive trials examining the optimal treatment for anal melanoma.
Reference
1. Kohli S, Narang S, Singhal A, Kumar V, Kaur O, Chandoke R. Malignant melanoma of the rectum. J Clin Imaging Sci. 2014;4:4. Published 2014 Jan 30. doi:10.4103/2156-7514.126031
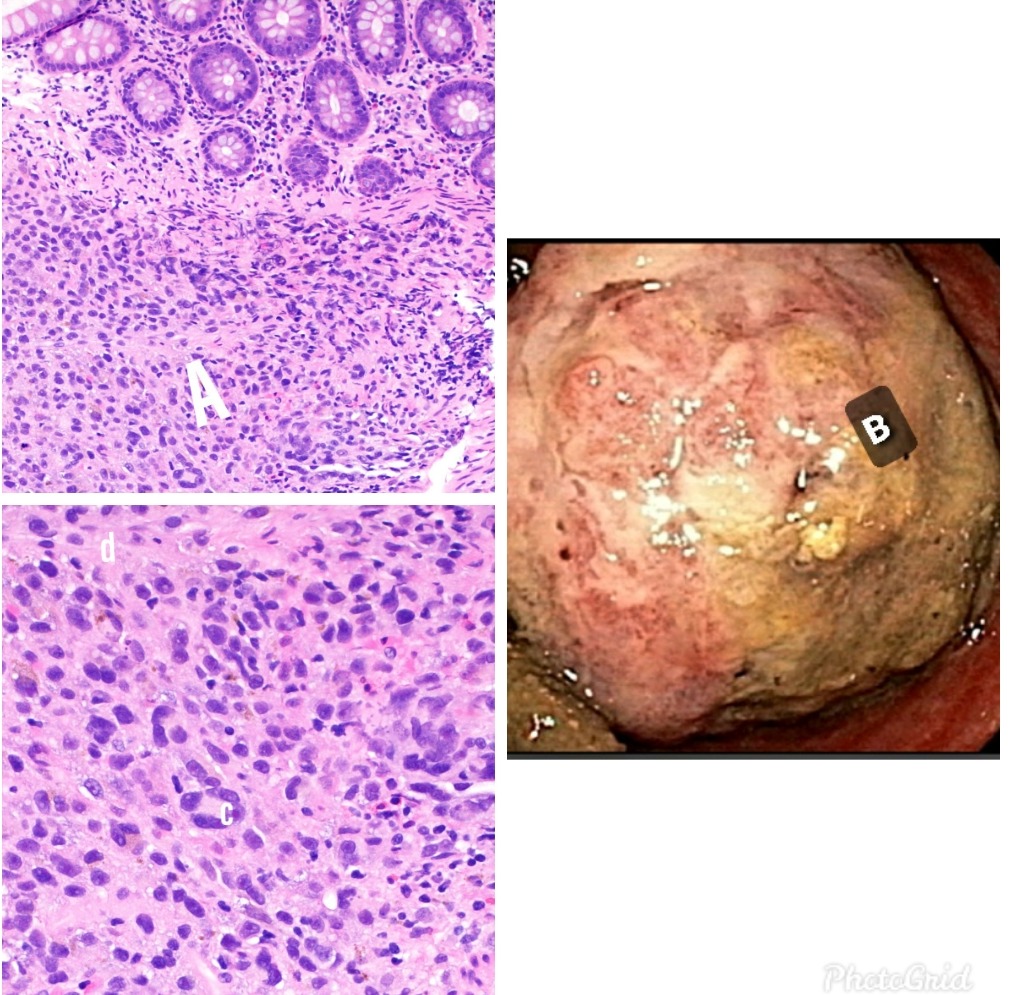
Figure: Fig A: Submucosal melanoma. Fig B: Rectal mass seen with colonoscope retroflexion. Fig c: Atypical melanocyte with prominent macronuclei. Fig d: Cytoplasmic pigment.
Disclosures:
Onyinye Ugonabo indicated no relevant financial relationships.
Mujtaba Mohamed indicated no relevant financial relationships.
Ebubechukwu Ezeh indicated no relevant financial relationships.
Pramod Pantangi indicated no relevant financial relationships.
Shima Ghavimi indicated no relevant financial relationships.
Onyinye Ugonabo, MD1, Mujtaba Mohamed, MD1, Ebubechukwu Ezeh, MD2, Pramod Pantangi, MD1, Shima Ghavimi, MD3. A0106 - A Rare Case of Metastatic Primary Rectal Melanoma in a Geriatric Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
