Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0560 - Pseudo-Cirrhosis Secondary to Metastatic Breast Carcinoma Causing Sinusoidal Obstruction
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- AM
Adil S. Mir, MD
Virginia Tech Carilion School of Medicine, VA
Presenting Author(s)
Adil S. Mir, MD1, Diana Dougherty, MD1, Kristin Newman, PA-C2, Robert D. Moylan, MD, PhD3, David Lebel, MD1, Douglas Grider, MD1
1Virginia Tech Carilion School of Medicine, Roanoke, VA; 2Carilion Clinic, Roanoke, VA; 3Virginia Tech Carilion, Roanoke, VA
Introduction: Pseudo-cirrhosis Secondary to Metastatic Breast Carcinoma Causing Sinusoidal Obstruction
Case Description/Methods: 70-year-old female with past history of colonic adenocarcinoma, hemicolectomy presented with acute abdominal pain and distension. Labs showed AST 387 IU/L, ALT 167 IU/L, alkaline phosphatase 546 IU/L, total bilirubin 2.5 and direct 1.1 mg/dl (no past history of liver disease, previously normal LFTs), negative acute viral hepatitis panel. Computed tomography (CT) abdomen and pelvis without contrast showed normal liver without focal lesions, mildly enlarged spleen and moderate ascites. Diagnostic paracentesis was negative for spontaneous bacterial peritonitis, with serum-to-ascites albumin gradient (SAAG ) >1.1 and total protein 1.2 g/dl. Surgical cytology from the ascitic fluid was negative for metastatic disease. Magnetic resonance imaging (MRI) abdomen: unremarkable liver, gall bladder and biliary system. 2D echocardiogram showed no acute abnormalities. Abdominal veins duplex showed hepato-fugal flow in the main portal vein but normal flow in the hepatic vein and inferior vena cava. A diagnostic liver biopsy was obtained (porto-systemic gradient = 26 mmHg)
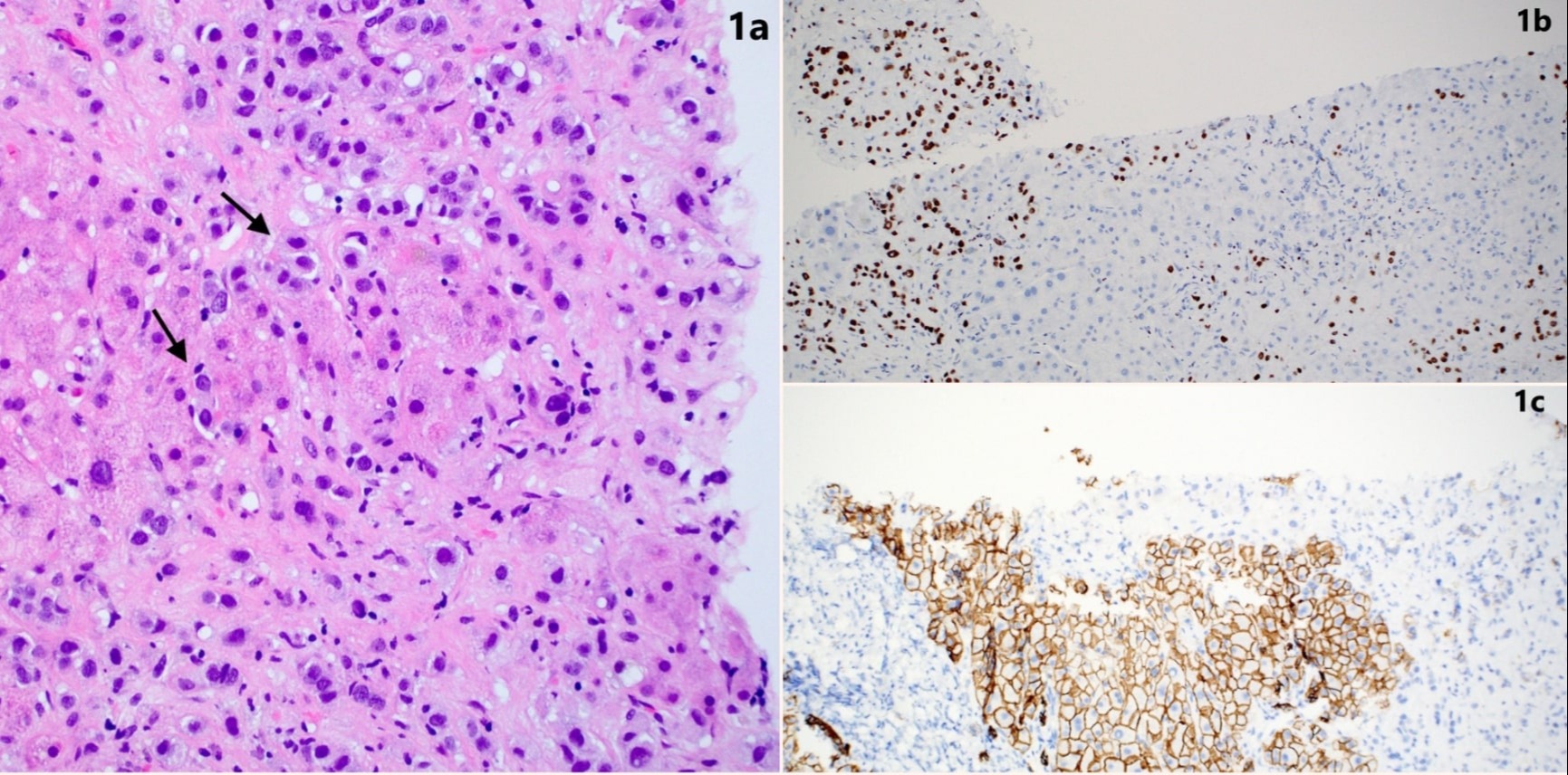
Histopathology revealed the initial presentation of ductal breast carcinoma metastatic to the liver, poorly differentiated involving portal areas and filing the sinusoids (Figure 1a). The carcinoma was keratin CAM5.2, CK7, GATA3 ( Figure 1b), mammaglobin, and BRST-2 positive, confirming metastatic breast carcinoma; the positive e-cadherin (Figure 1c) stain helps confirm ductal phenotype. Negative stains included CDX-2 and villin, helping to exclude a colorectal primary. Napsin-A and TTF-1 were negative, helping to exclude a pulmonary adenocarcinoma. Arginase 1 negative suggesting against a poorly differentiated hepatocellular carcinoma. Masson-trichrome/ reticulin stains showed pseudo-cirrhotic pattern with many hepatocytes separated by fibrosis along with infiltration of large numbers of tumor cells. The carcinoma was noted to be Her2/Neu, quantitative estrogen and progesterone receptor staining negative (Triple negative)
Discussion: The possibility of microscopic tumoral sinusoidal obstruction should always be in the clinical and histopathologic differential diagnosis in patients presenting with acute hepatitis and portal hypertensive features, especially ascites.
Disclosures:
Adil S. Mir, MD1, Diana Dougherty, MD1, Kristin Newman, PA-C2, Robert D. Moylan, MD, PhD3, David Lebel, MD1, Douglas Grider, MD1. E0560 - Pseudo-Cirrhosis Secondary to Metastatic Breast Carcinoma Causing Sinusoidal Obstruction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Virginia Tech Carilion School of Medicine, Roanoke, VA; 2Carilion Clinic, Roanoke, VA; 3Virginia Tech Carilion, Roanoke, VA
Introduction: Pseudo-cirrhosis Secondary to Metastatic Breast Carcinoma Causing Sinusoidal Obstruction
Case Description/Methods: 70-year-old female with past history of colonic adenocarcinoma, hemicolectomy presented with acute abdominal pain and distension. Labs showed AST 387 IU/L, ALT 167 IU/L, alkaline phosphatase 546 IU/L, total bilirubin 2.5 and direct 1.1 mg/dl (no past history of liver disease, previously normal LFTs), negative acute viral hepatitis panel. Computed tomography (CT) abdomen and pelvis without contrast showed normal liver without focal lesions, mildly enlarged spleen and moderate ascites. Diagnostic paracentesis was negative for spontaneous bacterial peritonitis, with serum-to-ascites albumin gradient (SAAG ) >1.1 and total protein 1.2 g/dl. Surgical cytology from the ascitic fluid was negative for metastatic disease. Magnetic resonance imaging (MRI) abdomen: unremarkable liver, gall bladder and biliary system. 2D echocardiogram showed no acute abnormalities. Abdominal veins duplex showed hepato-fugal flow in the main portal vein but normal flow in the hepatic vein and inferior vena cava. A diagnostic liver biopsy was obtained (porto-systemic gradient = 26 mmHg)
Histopathology revealed the initial presentation of ductal breast carcinoma metastatic to the liver, poorly differentiated involving portal areas and filing the sinusoids (Figure 1a). The carcinoma was keratin CAM5.2, CK7, GATA3 ( Figure 1b), mammaglobin, and BRST-2 positive, confirming metastatic breast carcinoma; the positive e-cadherin (Figure 1c) stain helps confirm ductal phenotype. Negative stains included CDX-2 and villin, helping to exclude a colorectal primary. Napsin-A and TTF-1 were negative, helping to exclude a pulmonary adenocarcinoma. Arginase 1 negative suggesting against a poorly differentiated hepatocellular carcinoma. Masson-trichrome/ reticulin stains showed pseudo-cirrhotic pattern with many hepatocytes separated by fibrosis along with infiltration of large numbers of tumor cells. The carcinoma was noted to be Her2/Neu, quantitative estrogen and progesterone receptor staining negative (Triple negative)
Discussion: The possibility of microscopic tumoral sinusoidal obstruction should always be in the clinical and histopathologic differential diagnosis in patients presenting with acute hepatitis and portal hypertensive features, especially ascites.
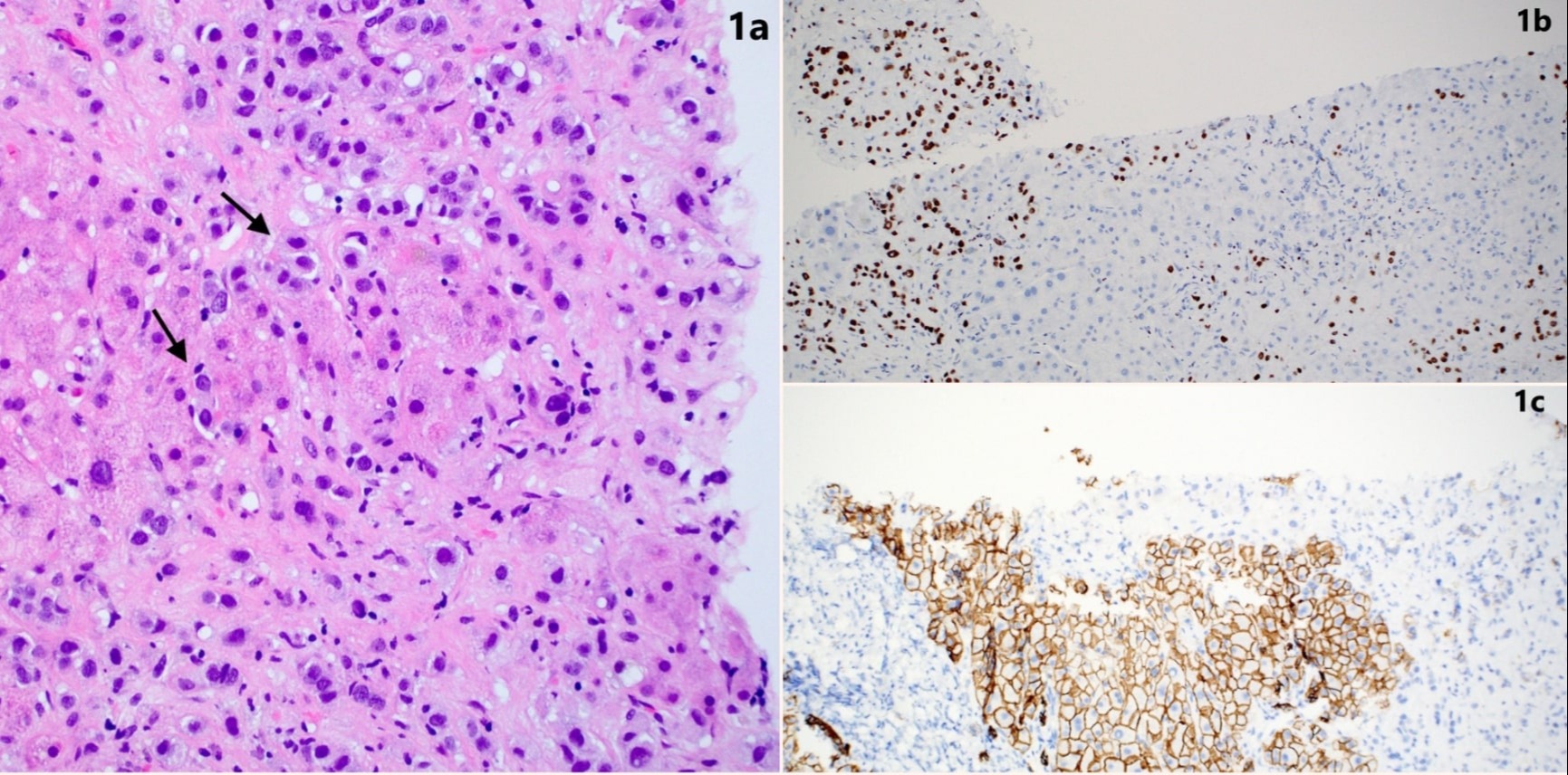
Figure: Figure 1. (a) H&E, 20X, Arrows show carcinoma in the sinusoids causing obstruction (b) GATA3, 10X (c) E-cadherin, 10X
Disclosures:
Adil Mir indicated no relevant financial relationships.
Diana Dougherty indicated no relevant financial relationships.
Kristin Newman indicated no relevant financial relationships.
Robert Moylan indicated no relevant financial relationships.
David Lebel indicated no relevant financial relationships.
Douglas Grider indicated no relevant financial relationships.
Adil S. Mir, MD1, Diana Dougherty, MD1, Kristin Newman, PA-C2, Robert D. Moylan, MD, PhD3, David Lebel, MD1, Douglas Grider, MD1. E0560 - Pseudo-Cirrhosis Secondary to Metastatic Breast Carcinoma Causing Sinusoidal Obstruction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
