Back

Poster Session B - Monday Morning
Category: Small Intestine
B0664 - Whipple’s Disease Without Arthropathy in an Immunocompromised Patient
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Ayham Khrais, DO
Rutgers New Jersey Medical School
West Orange, New Jersey
Presenting Author(s)
Ayham Khrais, DO1, Bing Han, MD2, Dhanasekaran Ramasamy, MD3, Shiva Kumar, MD4
1Rutgers New Jersey Medical School, West Orange, NJ; 2Cooperman Barnabas Medical Center, Livingston, NJ; 3Center for Digestive Diseases, Union, NJ; 4Digestive Disease Institute at Cleveland Clinic Abu Dhabi, Abu Dhabi, Abu Dhabi, United Arab Emirates
Introduction: Whipple’s disease (WD) is a rare disorder caused by the pathogen Tropheryma whipplei. It presents with non-specific symptoms which can mimic the presentation of other gastrointestinal pathogens, especially in immunocompromised patients. We report a unique presentation of WD involving an immunocompromised patient who experienced non-specific gastrointestinal symptoms without arthralgia, which is a characteristic symptom of this disease.
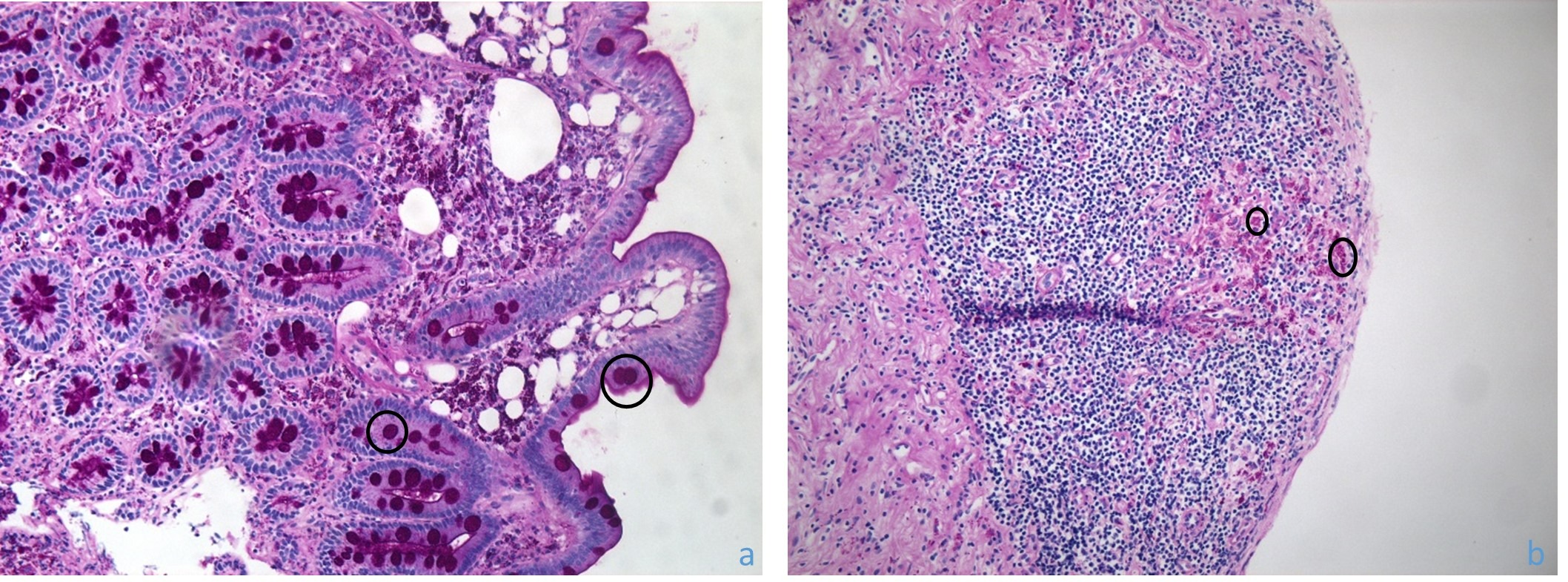
Case Description/Methods: A 67-year-old man with a history of chronic hepatitis B infection and Human immunodeficiency virus (HIV) infection presented with weight loss, nausea, vomiting and myalgia. Of note, patient did not have arthralgia. Physical exam revealed cervical lymphadenopathy and diffuse abdominal tenderness. Patient was anemic (hemoglobin of 8.6 g/dL) with a normal white count. Endoscopy demonstrated erythema in the gastric body, lymphangiectasia of the duodenum, and increased granularity of the terminal ileum. Mucosal biopsies revealed macrophages in the lamina propria with focal histiocytic aggregates throughout the small bowel and cecum, with positive PAS staining, consistent with Whipple’s disease. Confirmatory T. whipplei PCR testing was positive.
Discussion: WD is a rare diagnosis that must be considered in the differential diagnoses of patients presenting with unexplained nausea, vomiting, diarrhea and anemia. Furthermore, in patients with HIV, the possibilities would also include opportunistic gastrointestinal pathogens. Classic WD is characterized by diarrhea, weight loss, abdominal pain and extra-intestinal involvement manifesting as joint pain, endocarditis, dementia, supranuclear gaze palsy, and mediastinal lymphadenopathy. Diagnosis involves biopsy of affected tissue demonstrating foamy macrophages with PAS (+) substance, which can be confirmed by PCR or immunohistochemistry. Treatment involves an initial course of penicillin or ceftriaxone followed by a prolonged course of Bactrim, or a one-year course of doxycycline and hydroxychloroquine, followed by lifelong doxycycline therapy, which is more likely to prevent disease relapse. In the absence of suppressive therapy, relapse of WD is common and may lead to further complications, including neurological involvement.
Disclosures:
Ayham Khrais, DO1, Bing Han, MD2, Dhanasekaran Ramasamy, MD3, Shiva Kumar, MD4. B0664 - Whipple’s Disease Without Arthropathy in an Immunocompromised Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Rutgers New Jersey Medical School, West Orange, NJ; 2Cooperman Barnabas Medical Center, Livingston, NJ; 3Center for Digestive Diseases, Union, NJ; 4Digestive Disease Institute at Cleveland Clinic Abu Dhabi, Abu Dhabi, Abu Dhabi, United Arab Emirates
Introduction: Whipple’s disease (WD) is a rare disorder caused by the pathogen Tropheryma whipplei. It presents with non-specific symptoms which can mimic the presentation of other gastrointestinal pathogens, especially in immunocompromised patients. We report a unique presentation of WD involving an immunocompromised patient who experienced non-specific gastrointestinal symptoms without arthralgia, which is a characteristic symptom of this disease.
Case Description/Methods: A 67-year-old man with a history of chronic hepatitis B infection and Human immunodeficiency virus (HIV) infection presented with weight loss, nausea, vomiting and myalgia. Of note, patient did not have arthralgia. Physical exam revealed cervical lymphadenopathy and diffuse abdominal tenderness. Patient was anemic (hemoglobin of 8.6 g/dL) with a normal white count. Endoscopy demonstrated erythema in the gastric body, lymphangiectasia of the duodenum, and increased granularity of the terminal ileum. Mucosal biopsies revealed macrophages in the lamina propria with focal histiocytic aggregates throughout the small bowel and cecum, with positive PAS staining, consistent with Whipple’s disease. Confirmatory T. whipplei PCR testing was positive.
Discussion: WD is a rare diagnosis that must be considered in the differential diagnoses of patients presenting with unexplained nausea, vomiting, diarrhea and anemia. Furthermore, in patients with HIV, the possibilities would also include opportunistic gastrointestinal pathogens. Classic WD is characterized by diarrhea, weight loss, abdominal pain and extra-intestinal involvement manifesting as joint pain, endocarditis, dementia, supranuclear gaze palsy, and mediastinal lymphadenopathy. Diagnosis involves biopsy of affected tissue demonstrating foamy macrophages with PAS (+) substance, which can be confirmed by PCR or immunohistochemistry. Treatment involves an initial course of penicillin or ceftriaxone followed by a prolonged course of Bactrim, or a one-year course of doxycycline and hydroxychloroquine, followed by lifelong doxycycline therapy, which is more likely to prevent disease relapse. In the absence of suppressive therapy, relapse of WD is common and may lead to further complications, including neurological involvement.
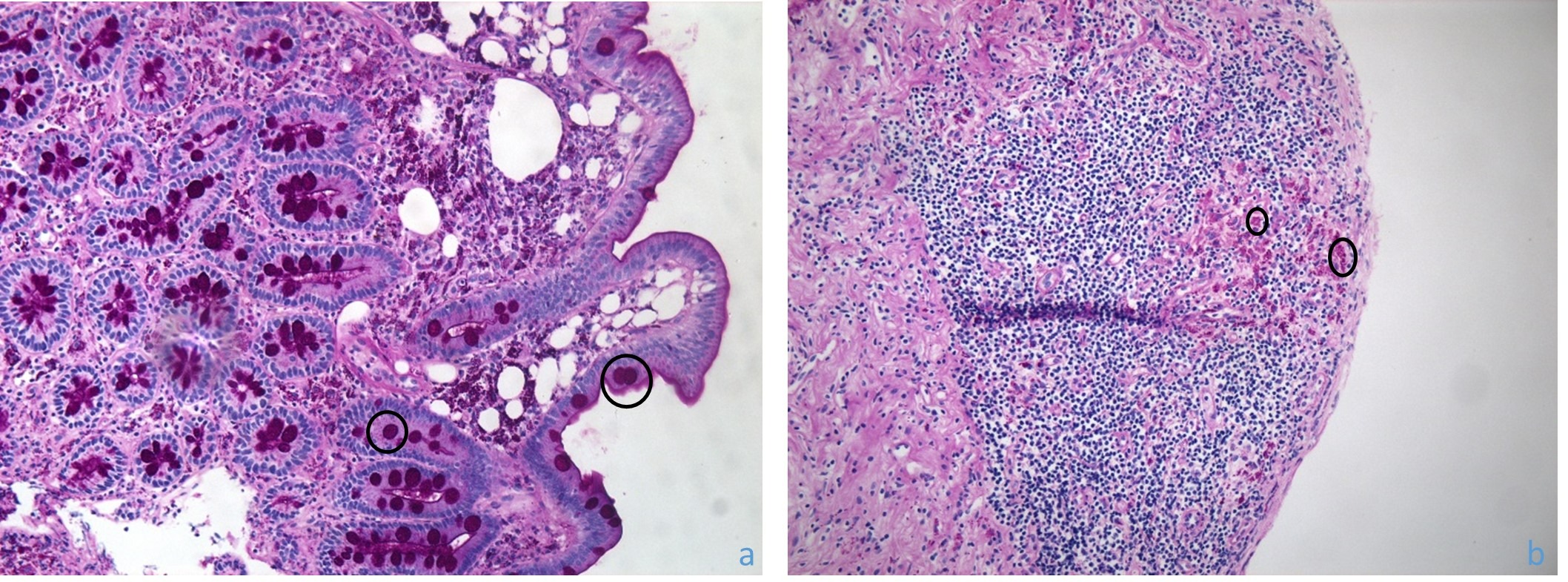
Figure: Figure 1 Periodic Acid-Schiff-Staining Macrophages (circles) Within the Lamina Propria of the Duodenal Bulb (a) and Cecum (b) as Seen Via Light Microscopy with a 20x Objective Lens.
Disclosures:
Ayham Khrais indicated no relevant financial relationships.
Bing Han indicated no relevant financial relationships.
Dhanasekaran Ramasamy indicated no relevant financial relationships.
Shiva Kumar indicated no relevant financial relationships.
Ayham Khrais, DO1, Bing Han, MD2, Dhanasekaran Ramasamy, MD3, Shiva Kumar, MD4. B0664 - Whipple’s Disease Without Arthropathy in an Immunocompromised Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
