Back

Poster Session B - Monday Morning
Category: GI Bleeding
B0348 - Obscure GI Bleed From Metastatic Melanoma
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Umer Ejaz Malik, MD
Albany Medical Center
Albany, NY
Presenting Author(s)
Umer Ejaz Malik, MD, Joo Hye Park, MD, Maria Faraz, MBBS, Stephen Hasak, MD, MPH
Albany Medical Center, Albany, NY
Introduction: Malignant melanona is an epithelial cancer arising from melanocytes. GI tract is usual site of involvement in patients with metastasis. We present a patient who presented with a GI bleed and was diagnosed to have metastatic gastric melanoma.
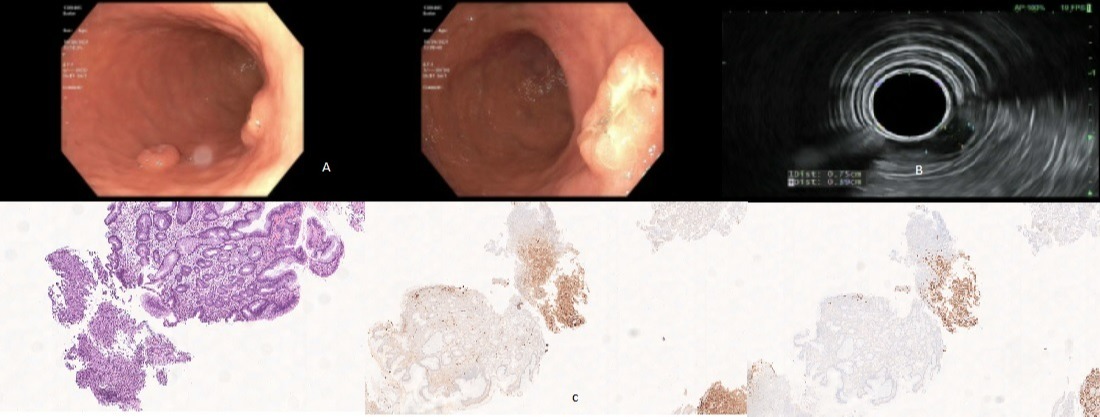
Case Description/Methods: 84 year old female with PMH of atrial fibrillation, on Eliquis was recently diagnosed with melanoma in right upper extremity and regional axillary lymphadenopathy. Patient had undergone wide local excision with adjuvant Pembrolizumab. On follow up visit with oncology, patient reported having fatigue. Lab work up showed anemia with Hgb of 5.5 g/dl (baseline 13 g/dl). She was hospitalized and received blood transfusions which resulted in improvement of her Hgb. GI service was consulted. On evaluation, patient reported having mild epigastric pain and melena. ROS was unremarkable. She was scheduled for an EGD. EGD showed two 10 mm submucosal nodules in stomach with central ulceration (A) along with duodenal erosions with unremarkable esophagus. There was no evidence of fresh or old bleeding. Patient was scheduled for an EUS for further evaluation of gastric lesions. A colonoscopy was also scheduled to determine cause of GI bleed. EUS was performed which showed evidence of two ulcerated intramural (subepithelial) lesions in the body and at incisura of the stomach. These lesions were hypoechoic and heterogenous. These lesions appeared to originate from the deep mucosa (layer 2) measuring 5 mm in maximum thickness with well defined outer borders (B). Sonographic findings were considered to be consisted with aberrant pancreas versus metastasis. FNB was performed. Colonoscopy was unremarkable other than diverticulosis and internal hemorrhoids. Subsequent lab work showed stable blood counts without need for any further blood transfusion. Anticoagulation was resumed on discharge. Biopsy showed presence of tumors cells diffusely positive for SOX10 and S100 and negative for MNF116. These were considered to be related to metastatic melanoma (C). Follow up with oncology was established on discharge to discuss further management.
Discussion: Malignant melanoma is commonly associated with metastasis with involvement of GI tract with 23% with gastric involvement, commonly presenting with abdominal pain and GI bleeds. Prognosis is usually poor with median survival reported upto 6-8 months. Treatment involves surgical resection, chemotherapy or immunotherapy. Use of BRAF targeted therapies and immune checkpoint inhibitors have increased survival rates.
Disclosures:
Umer Ejaz Malik, MD, Joo Hye Park, MD, Maria Faraz, MBBS, Stephen Hasak, MD, MPH. B0348 - Obscure GI Bleed From Metastatic Melanoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Albany Medical Center, Albany, NY
Introduction: Malignant melanona is an epithelial cancer arising from melanocytes. GI tract is usual site of involvement in patients with metastasis. We present a patient who presented with a GI bleed and was diagnosed to have metastatic gastric melanoma.
Case Description/Methods: 84 year old female with PMH of atrial fibrillation, on Eliquis was recently diagnosed with melanoma in right upper extremity and regional axillary lymphadenopathy. Patient had undergone wide local excision with adjuvant Pembrolizumab. On follow up visit with oncology, patient reported having fatigue. Lab work up showed anemia with Hgb of 5.5 g/dl (baseline 13 g/dl). She was hospitalized and received blood transfusions which resulted in improvement of her Hgb. GI service was consulted. On evaluation, patient reported having mild epigastric pain and melena. ROS was unremarkable. She was scheduled for an EGD. EGD showed two 10 mm submucosal nodules in stomach with central ulceration (A) along with duodenal erosions with unremarkable esophagus. There was no evidence of fresh or old bleeding. Patient was scheduled for an EUS for further evaluation of gastric lesions. A colonoscopy was also scheduled to determine cause of GI bleed. EUS was performed which showed evidence of two ulcerated intramural (subepithelial) lesions in the body and at incisura of the stomach. These lesions were hypoechoic and heterogenous. These lesions appeared to originate from the deep mucosa (layer 2) measuring 5 mm in maximum thickness with well defined outer borders (B). Sonographic findings were considered to be consisted with aberrant pancreas versus metastasis. FNB was performed. Colonoscopy was unremarkable other than diverticulosis and internal hemorrhoids. Subsequent lab work showed stable blood counts without need for any further blood transfusion. Anticoagulation was resumed on discharge. Biopsy showed presence of tumors cells diffusely positive for SOX10 and S100 and negative for MNF116. These were considered to be related to metastatic melanoma (C). Follow up with oncology was established on discharge to discuss further management.
Discussion: Malignant melanoma is commonly associated with metastasis with involvement of GI tract with 23% with gastric involvement, commonly presenting with abdominal pain and GI bleeds. Prognosis is usually poor with median survival reported upto 6-8 months. Treatment involves surgical resection, chemotherapy or immunotherapy. Use of BRAF targeted therapies and immune checkpoint inhibitors have increased survival rates.
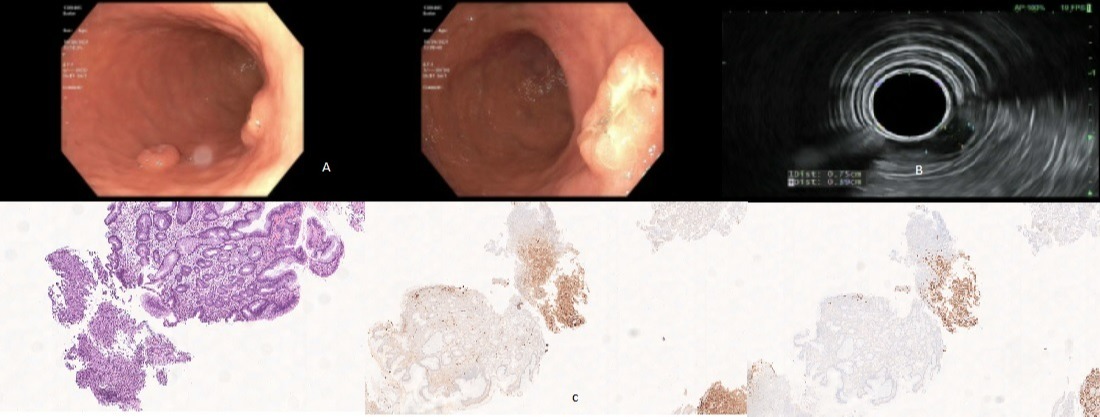
Figure: A: Submucosal lesions B: EUS findings C: Metastatic melanoma with positive SOX-10 and S100.
Disclosures:
Umer Ejaz Malik indicated no relevant financial relationships.
Joo Hye Park indicated no relevant financial relationships.
Maria Faraz indicated no relevant financial relationships.
Stephen Hasak indicated no relevant financial relationships.
Umer Ejaz Malik, MD, Joo Hye Park, MD, Maria Faraz, MBBS, Stephen Hasak, MD, MPH. B0348 - Obscure GI Bleed From Metastatic Melanoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

