Back

Poster Session B - Monday Morning
Category: Liver
B0573 - Recurrent Liver Abscess in a Non-Toxic Patient
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Ayham Khrais, DO
Rutgers New Jersey Medical School
West Orange, New Jersey
Presenting Author(s)
Ayham Khrais, DO1, Ahmad Ali, MD2, Catherine Choi, MD2, Siddharth Verma, DO2
1Rutgers New Jersey Medical School, West Orange, NJ; 2Rutgers New Jersey Medical School, Newark, NJ
Introduction: Liver abscesses are caused by direct spread from peritonitis, biliary tract infection or via hematogenous seeding from a distant source. Most are polymicrobial, however Escherichia coli and Klebsiella pneumoniae are the most common offending pathogens. Patients usually present with pain, fever, and clinical signs of infection. We describe a case of spontaneous liver abscess in a non-toxic patient that recurred 10 years after a previous abscess.
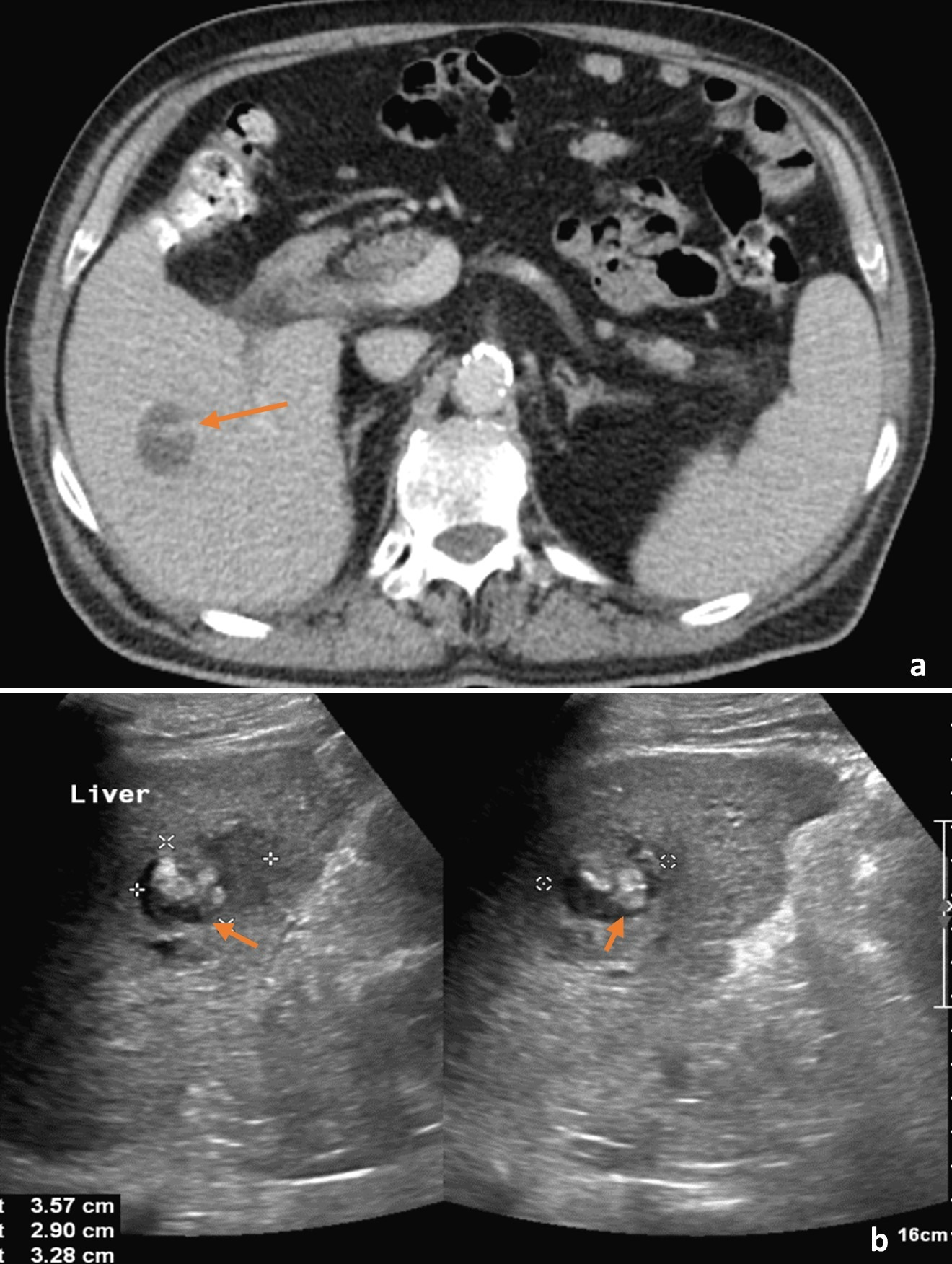
Case Description/Methods: Case Description/Methods: A 73-year-old-man with a history of type 2 diabetes mellitus, hypertension, CAD status post CABG and PCI 3 years ago, and abdominal aortic aneurysm status post endovascular aneurysm repair presented with 2 weeks of dark urine. After receiving his COVID-19 booster and influenza vaccinations, he developed flu-like symptoms with a self-resolving fever of 101.8°F. He had dark amber urine without dysuria or hematuria. Later, he experienced generalized weakness and decreased oral intake. Outpatient labs showed elevated liver function tests, and he was told to present to the ED. On arrival, he was afebrile with stable vitals. Physical exam was unremarkable. Laboratory evaluation showed a hemoglobin of 11.7 g/dL, sodium of 133 mEq/L, creatinine of 1.4 mg/dL, aspartate aminotransferase of 117 U/L, alanine aminotransferase of 212 U/L, alkaline phosphatase of 825 U/L, total bilirubin of 4.1 mg/dL, and direct bilirubin of 2.1 mg/dL. Triple-phase CT showed a 2.8 cm mass in the right liver lobe with linear enhancement. Ultrasound showed mixed echogenicity measuring 3.6 x 2.9 x 3.3 cm in segment 8 of the liver. On further evaluation, patient had an E. coli abscess diagnosed 10 years prior, managed with antibiotics and drainage. At that time, the abscess was within the right inferior liver lobe, similar to his current abscess. LFTs downtrended. Abscess was aspirated, with culture growing oxidase negative, gram-negative rods, likely E. coli. Patient started on ceftriaxone and metronidazole, to undergo colonoscopy as an outpatient and rule out colonic bacterial translocation.
Discussion: Pyogenic liver abscess can result in significant morbidity and mortality because of worsening infection and sepsis. Abscesses occur because of spread from adjacent infection or after recent surgeries. Recurrence is very rare. Here, we describe a very unusual case of a pyogenic liver abscess growing E. coli in a non-toxic patient, with the same location and causative organism as an abscess managed 10 years prior.
Disclosures:
Ayham Khrais, DO1, Ahmad Ali, MD2, Catherine Choi, MD2, Siddharth Verma, DO2. B0573 - Recurrent Liver Abscess in a Non-Toxic Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Rutgers New Jersey Medical School, West Orange, NJ; 2Rutgers New Jersey Medical School, Newark, NJ
Introduction: Liver abscesses are caused by direct spread from peritonitis, biliary tract infection or via hematogenous seeding from a distant source. Most are polymicrobial, however Escherichia coli and Klebsiella pneumoniae are the most common offending pathogens. Patients usually present with pain, fever, and clinical signs of infection. We describe a case of spontaneous liver abscess in a non-toxic patient that recurred 10 years after a previous abscess.
Case Description/Methods: Case Description/Methods: A 73-year-old-man with a history of type 2 diabetes mellitus, hypertension, CAD status post CABG and PCI 3 years ago, and abdominal aortic aneurysm status post endovascular aneurysm repair presented with 2 weeks of dark urine. After receiving his COVID-19 booster and influenza vaccinations, he developed flu-like symptoms with a self-resolving fever of 101.8°F. He had dark amber urine without dysuria or hematuria. Later, he experienced generalized weakness and decreased oral intake. Outpatient labs showed elevated liver function tests, and he was told to present to the ED. On arrival, he was afebrile with stable vitals. Physical exam was unremarkable. Laboratory evaluation showed a hemoglobin of 11.7 g/dL, sodium of 133 mEq/L, creatinine of 1.4 mg/dL, aspartate aminotransferase of 117 U/L, alanine aminotransferase of 212 U/L, alkaline phosphatase of 825 U/L, total bilirubin of 4.1 mg/dL, and direct bilirubin of 2.1 mg/dL. Triple-phase CT showed a 2.8 cm mass in the right liver lobe with linear enhancement. Ultrasound showed mixed echogenicity measuring 3.6 x 2.9 x 3.3 cm in segment 8 of the liver. On further evaluation, patient had an E. coli abscess diagnosed 10 years prior, managed with antibiotics and drainage. At that time, the abscess was within the right inferior liver lobe, similar to his current abscess. LFTs downtrended. Abscess was aspirated, with culture growing oxidase negative, gram-negative rods, likely E. coli. Patient started on ceftriaxone and metronidazole, to undergo colonoscopy as an outpatient and rule out colonic bacterial translocation.
Discussion: Pyogenic liver abscess can result in significant morbidity and mortality because of worsening infection and sepsis. Abscesses occur because of spread from adjacent infection or after recent surgeries. Recurrence is very rare. Here, we describe a very unusual case of a pyogenic liver abscess growing E. coli in a non-toxic patient, with the same location and causative organism as an abscess managed 10 years prior.
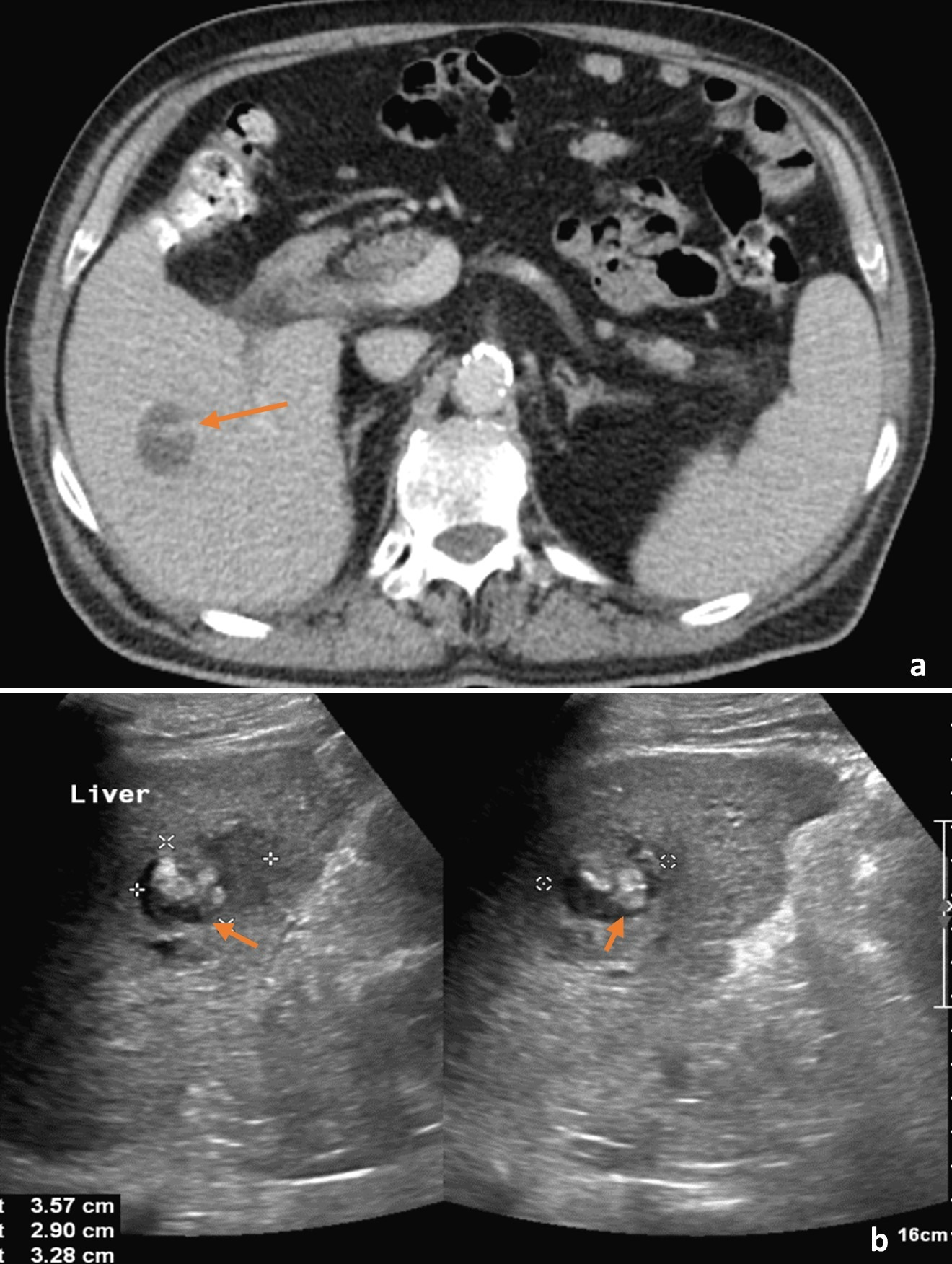
Figure: Figure 1 Triple phase CT scan of the abdomen and pelvis in the transverse plane (a) demonstrating a 2.8 cm mass (arrow) in the right lobe of the liver with a small area of linear enhancement. Abdominal ultrasound demonstrating an area of mixed echogenicity (arrows) with areas of increased and decreased sonographic texture measuring 3.6 x 2.9 x 3.3 cm in segment 8 of the liver (b).
CT: computed tomography.
CT: computed tomography.
Disclosures:
Ayham Khrais indicated no relevant financial relationships.
Ahmad Ali indicated no relevant financial relationships.
Catherine Choi indicated no relevant financial relationships.
Siddharth Verma indicated no relevant financial relationships.
Ayham Khrais, DO1, Ahmad Ali, MD2, Catherine Choi, MD2, Siddharth Verma, DO2. B0573 - Recurrent Liver Abscess in a Non-Toxic Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
