Category: Antimicrobial Stewardship: Trends in Antimicrobial Prescribing
Poster Session: Antimicrobial Stewardship: Trends in Antimicrobial Prescribing
237 - Inpatient and Discharge Antibiotic Use for Hospitalized Patients Growing Multi-Drug Resistant Bacteria in Urine Cultures
- JZ
James Zou
Resident Physician
Washington University School of Medicine at St. Louis / Barnes-Jewish Hospital
REDWOOD CITY, CaliforniaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- FB
Frances Boly
Infectious Diseases Fellow
Washington University School of Medicine at St. Louis / Barnes-Jewish Hospital
Saint Louis, MissouriDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- DS
Dustin Stwalley
Programmer Analyst
Washington University School of Medicine in St. Louis
Saint Louis, MissouriDisclosure: AbbVie Inc (Shareholder)Bristol-Myers Squibb (Shareholder)

Margaret A A. Olsen
Professor
Washington University School of Medicine
St. Louis, MissouriDisclosure: Merck (Grant/Research Support)Pfizer (Consultant, Grant/Research Support)
- JK
Jennie H. Kwon
Assistant Professor of Medicine
Washington University School of Medicine at St. Louis
Saint Louis, MissouriDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JB
Jason P. Burnham
Instructor of Medicine, Associate Hospital Epidemiologist
Washington University in St. Louis School of Medicine
St. Louis, MODisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
Presenting Author(s)
Co-Author(s)
Background:
Multidrug resistant organism (MDRO) infections are a threat to public health. Urinary tract infections (UTIs) are the most common MDRO infection and are responsible for a significant proportion of antibiotic use. Studies demonstrate both duration and type of antibiotics prescribed to patients with MDRO UTI are inappropriate, and that asymptomatic MDRO bacteriuria is inappropriately treated. In addition, antibiotics prescribed at hospital discharge are inappropriate in ~70% of patients. We sought to characterize inpatient and outpatient antibiotic durations to describe burden of antibiotic use for patients with an MDRO isolated from a urine specimen during a hospitalization.
Methods:
This retrospective study was conducted at Barnes-Jewish Hospital, a 1266-bed academic medical center in St. Louis, Missouri from 11/7/12-11/7/17. Patients ≥ 18 years of age were included if they had an MDRO isolated from a urine specimen and no other positive bacterial cultures during their hospitalization. Demographics, comorbidities, cultures, and antibiotics were collected via data pulls and chart review. MDROs were defined according to European and US Center for Disease Control and Prevention guidelines. Antibiotic use was described as percentages of all antibiotics used.
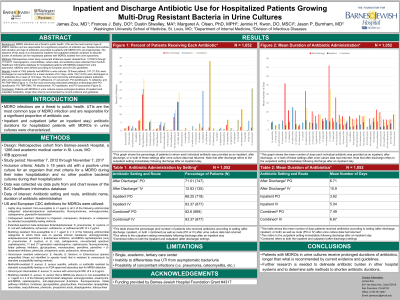
Results:
A total of 1052 patients had MDROs in urine cultures. Of these patients, 747 (71.0%) were discharged on oral antibiotics for a mean duration of 6.7 days, while 135 (12.8%) were discharged on IV antibiotics for a mean of 10.9 days. The five most commonly administered inpatient antibiotics after urine culture results were available (% prescribed) were IV ceftriaxone (43.0%), IV vancomycin (26.0%), PO ciprofloxacin (25.6%), IV cefepime (24.5%), and PO trimethoprim-sulfamethoxazole (17.6%). The five most commonly prescribed antibiotics at discharge were PO ciprofloxacin (22.3%), PO trimethoprim-sulfamethoxazole (17.8%), PO nitrofurantoin (8.4%), PO cephalexin (6.2%), and PO doxycycline (5.0%).
Conclusion: Patients with MDROs in urine cultures receive prolonged durations of inpatient and outpatient antibiotics, longer than what is recommended by current evidence and guidelines.

