Category: Infections in Immunocompromised Individuals
Poster Session: Infections in Immunocompromised Individuals
1080 - Changing Epidemiology and Long-Term Outcome of Bloodstream Infection Due to Enterococcus for Patients with Acute Leukemia: Impacts and Limitations on Strategy of Restricting Antibiotics

Raeseok Lee
Clinical assistant professor
Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- SC
Sung-Yeon Cho
Clinical Assistant Professor
Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: Gilead (Grant/Research Support, Speaker's Bureau)Merck Sharp & Dohme (Grant/Research Support, Speaker's Bureau)Pfizer (Grant/Research Support, Speaker's Bureau)
- DL
Dong-Gun Lee
Professor
The Catholic University of Korea, Seoul, South Korea
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- TN
Tae-hoon No
Clinical fellow
Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- SC
Su-Mi Choi
Professor
Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- SK
Si-Hyun Kim
Assistant Professor
Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JC
Jae-Ki Choi
Clinical Assistant Professor
Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- SP
Sun Hee Park
Professor
Division of Infectious Diseases, Department of Internal Medicine , The Catholic University of Korea, Seoul, Korea
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JC
Jung-Hyun Choi
Professor
Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JY
Jin-Hong Yoo
Professor
Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
Presenting Author(s)
Co-Author(s)
Background: Gastrointestinal dysbiosis due to antibiotics and mucosal injury by intensive chemotherapy are important risk factors for Enterococcal infection in patients with acute leukemia. However, there is still disagreement about trends of incidence and outcome of bloodstream infection (BSI) due to Enterococcus species. This study aimed to identify the changes in the epidemiology of Enterococcal BSI and to estimate the long-term impact of Enterococcal BSI on outcome in an acute leukemia cohort.
Methods:
All adult acute leukemia patients diagnosed with Enterococcal BSI (N = 512) between 2014 to 2018 at the Catholic Hematology Hospital were retrospectively reviewed. The incidence rate was compared with antibiotics use and multivariable models were used to estimate the impact of Enterococcal BSI on the outcome.
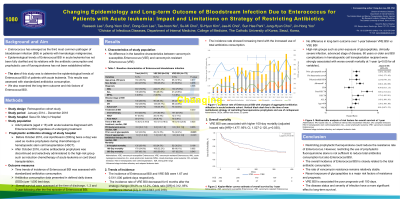
Results: Of 433 patients, 512 episodes of Enterococcal BSI occurred: 172 (33.6%) of 512 were vancomycin-resistant Enterococcus (VRE) and baseline characteristics were similar in comparison with vancomycin-susceptible Enterococcus (VSE) BSI. The incidence rate of VRE seemed to decrease for 6 months after a change in the strategy of restricting prophylactic use of fluoroquinolone and empirical use of carbapenem (39.2% vs 12.2%, Odds ratio [OR]=0.312, 95% confidence interval [CI], 0.116-0.843, p=0.018). However, overall Enterococcal BSI continued to increase with the rapidly increased use of unrestricted antibiotics. VRE BSI was associated with higher 100-day mortality than VSE BSI after adjusting for covariates (hazard ratio [HR]=1.477; 95% CI, 1.027-2.125, p=0.035), but there was no difference in long-term outcome at one year. In multivariable models, high-risk groups such as old age, advanced stage of disease, polymicrobial infection, high Pitt bacteremia score, and BSI complications after hematopoietic cell transplantation (HSCT) were strongly associated with worse long-term outcome (p< 0.05 for all variables).Table 1. Baseline characteristics of Enterococcal bloodstream infection (BSI).png) Figure 1. Incidence rate of Enterococcal BSI with changes of aggregated antibiotics utilization in acute leukemia cohort. Vertical black dash line is the time of new institutional strategy of restricting fluoroquinolone prophylaxis and use of carbapenem. Abbreviations: DDDs, defined daily doses; Q, quarter
Figure 1. Incidence rate of Enterococcal BSI with changes of aggregated antibiotics utilization in acute leukemia cohort. Vertical black dash line is the time of new institutional strategy of restricting fluoroquinolone prophylaxis and use of carbapenem. Abbreviations: DDDs, defined daily doses; Q, quarter.png) Figure 2. Multivariable analysis of risk factors for overall survival at one year. Abbreviations: HR, hazard ratio; CI, confidence interval; BSI, bloodstream infection; CR, complete remission; HSCT, hematopoietic stem cell transplantation; ALL, acute lymphocytic leukemia; VRE, vancomycin-resistant Enterococcus
Figure 2. Multivariable analysis of risk factors for overall survival at one year. Abbreviations: HR, hazard ratio; CI, confidence interval; BSI, bloodstream infection; CR, complete remission; HSCT, hematopoietic stem cell transplantation; ALL, acute lymphocytic leukemia; VRE, vancomycin-resistant Enterococcus.png)
Conclusion: The effort to restrict the use of fluoroquinolone and carbapenem alone is insufficient to reduce Enterococcal BSI. To improve long-term outcomes, especially in high-risk patients, multidisciplinary interventions to reduce the overall use of antibiotics along with the total incidence of Enterococcal BSI are needed.

