76 - Effect of Early Administration of Systemic Corticosteroids on Outcomes in Patients with COVID-19 Pneumonia
Background:
Systemic corticosteroids (steroids) have been empirically used in acute respiratory distress syndrome, an entity also present in coronavirus disease 19 (COVID-19). Early steroids administration could accelerate resolution of symptoms and reduce intensive care unit (ICU) stay in these patients, but practice varies widely as evidence is scant.
Methods: We reviewed the records of 498 adults admitted to Stony Brook University Hospital, NY, from 3/1 to 4/15, 2020 with COVID-19 requiring high-flow O2 (non-rebreather mask, Venturi mask with FiO2 >50%, or high-flow nasal cannula). We excluded those (N=29) who received mechanical ventilation (MV) or died within 24h of admission. We followed patients until death or discharge. We compared outcomes between patients who received early steroids (i.e. prior to MV) and those who did not. We used adjusted Cox models to evaluate the composite of death or need for MV. We also evaluated healthcare resources utilization.
Results: Of 469 patients, 175 (37.3%) received steroids while on high flow O2. Table 1 summarizes the baseline characteristics. Patients who received steroids were more likely to have asthma, had slightly longer duration of symptoms, lower O2 saturation, higher NT-proBNP and lower IL-6 levels at baseline. In total, 228 patients (48.6%) reached the composite endpoint (123 died and 105 received MV). By 7 days, 32.5% of patients who received steroids died or were intubated vs. 44.8% of those who did not (log-rank P=0.008), Figure 1. In models adjusted for race, age, sex, comorbidities, baseline O2 saturation and procalcitonin, steroids reduced risk for death or MV by 44% (hazard ratio [HR] 0.56; 95%CI 0.42–0.76; P< 0.001). The effect was time-dependent with initial HR 0.34 (95%CI 0.21–0.56; P< 0.001) and daily attenuation by 10.2% (95%CI 1.7%–19.4%; P=0.017). Mortality at 7 and 14 days did not differ between groups (8.1% vs. 8.3% and 19.1% vs. 21.0%, respectively, log-rank P=0.75). Among discharged patients, length of hospital stay was longer, but ICU stay was shorter with steroids, Table 2.Patient Characteristics According to Use of Early Steroids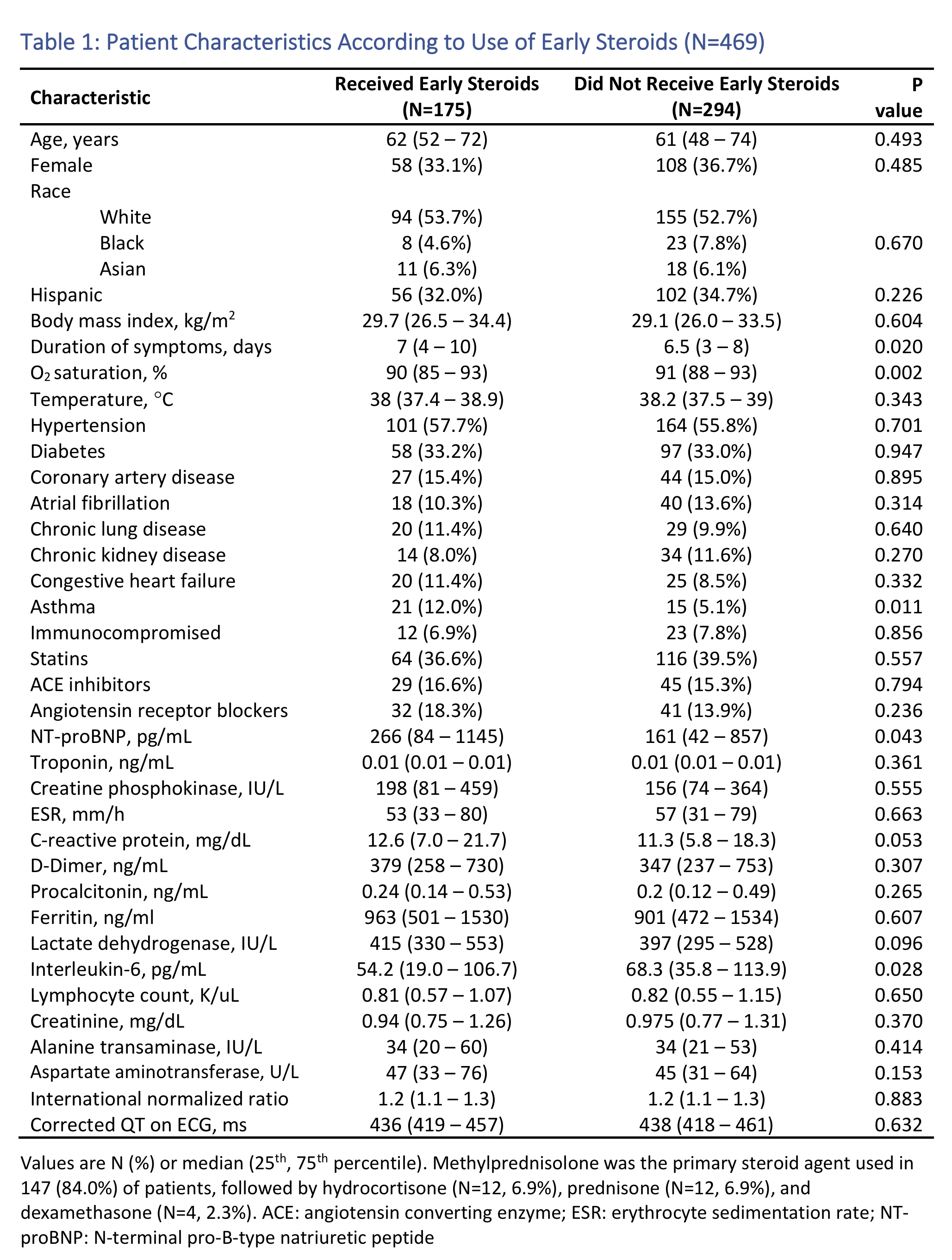 Kaplan-Meier Curves Based on Steroids Use for Death or Intubation
Kaplan-Meier Curves Based on Steroids Use for Death or Intubation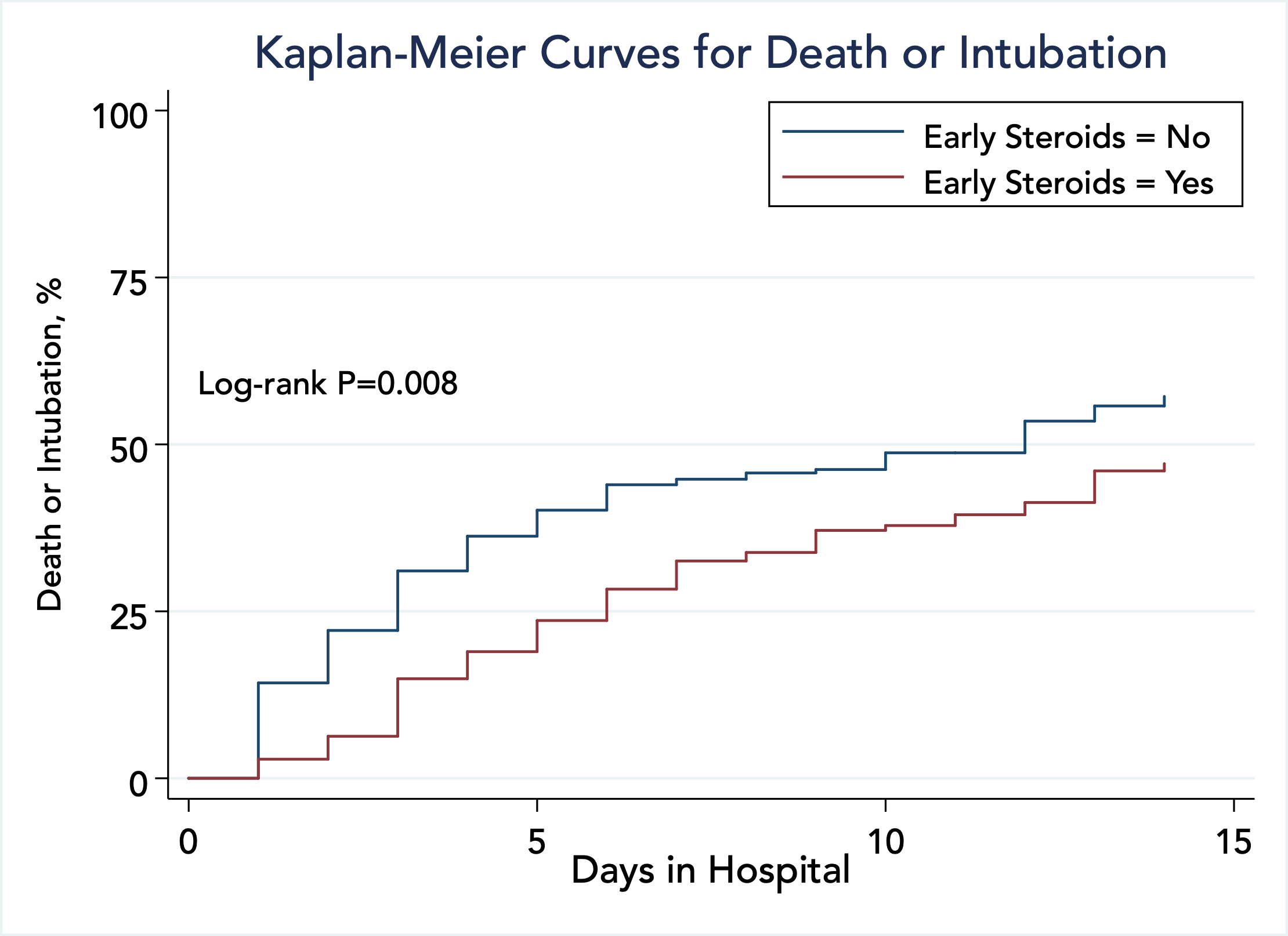 Healthcare Resources Utilization According to Use of Early Steroids Among Discharged Patients
Healthcare Resources Utilization According to Use of Early Steroids Among Discharged Patients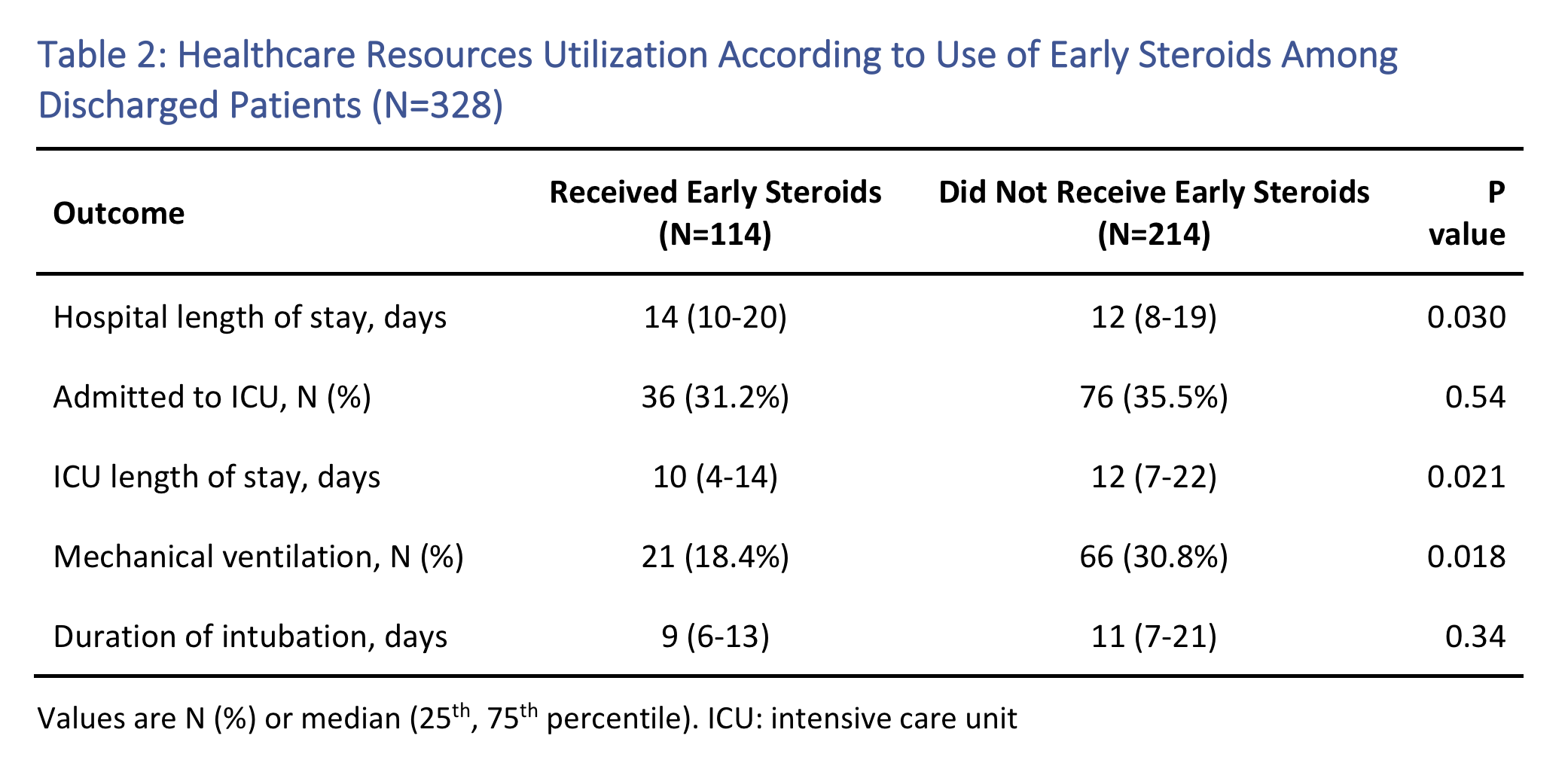
Conclusion: Early administration of steroids reduced primarily the need for MV in our high-risk COVID-19 patients, with shorter ICU utilization, at the expense of longer hospital stay. Further studies are needed to optimize the use of steroids in these patients.

Aikaterini Papamanoli, MD
Infectious Diseases Fellow
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- AK
Andreas Kalogeropoulos, MD, MPH, PhD
Associate Professor of Medicine (Cardiology)
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JF
Jenny Fung, BS
Medical Student
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JN
Jacquelyn Nakamura, BS
Medical Students
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JY
Jeanwoo Yoo, MD
Medical Resident
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- PG
Prabhjot Grewal, MD
Medical Resident
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- NK
Nikitha Karkala, BS
Medical Student
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JA
Joshua Abata, BS
Medical Student
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- ST
Stella T. Tsui, BS
Medical Student
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- AC
Alexandra Coritsidis, BS
Medical Student
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- AM
Azad Mojahedi, MD
Attending Physician
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- RJ
Robin Jacob, MD
Medical Resident
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JH
Jessica Hotelling, MD
Medical Resident
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- SD
Simrat Dhaliwal, BS
Medical Student
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- SR
Sahil Rawal, BS
medical Student
Stony Brook University Hospital
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- LM
Luis Marcos, MD, MPH
Associate Professor of Medicine, ID fellowship program director
Stony Brook University
Stony Brook, New YorkDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.


