Category: Treatment of Antimicrobial Resistant Infections
Poster Session: Treatment of Antimicrobial Resistant Infections
1592 - Antimicrobial Activity of Ceftazidime-Avibactam and Comparator Agents Against Enterobacterales and Pseudomonas aeruginosa With Overexpression of AmpC β-Lactamase From Phase 3 Clinical Trials

- DD
- WC
- UR
Presenting Author(s)
Co-Author(s)
Background: AmpC overproduction is a main mechanism of carbapenem resistance, in the absence of acquired carbapenemases. Ceftazidime-avibactam (CAZ-AVI) has potent in vitro activity against AmpC-producing P. aeruginosa and Enterobacterales that are resistant to carbapenems and other β-lactams.
Methods: Activity of CAZ-AVI and comparators was evaluated against AmpC-overproducing Enterobacterales (n=77) and P. aeruginosa (n=53) collected from 4 CAZ-AVI clinical trials: RECLAIM (complicated intra-abdominal infection [cIAI]), REPRISE (cIAI/complicated urinary tract infection [cUTI]), RECAPTURE (cUTI) and REPROVE (hospital-acquired pneumonia/ventilator associated pneumonia). In vitro susceptibility of CAZ-AVI and comparators was performed by broth microdilution using ThermoFisher custom panels. CLSI breakpoints were used to determine susceptibility. Quantitative PCR and microarray data were used to characterize presence and expression of AmpC. Clinical response at test of cure was assessed.
Results: Against 77 AmpC-overproducing Enterobacterales isolates, meropenem-vaborbactam (MVB) (98.7% susceptible [S]), CAZ-AVI (96.1% S), and meropenem (MEM) (96.1% S) had similar in vitro activity (Table), with greater in vitro activity than amikacin (AMK) (84.4% S), gentamicin (61.0% S), and ceftolozane-tazobactam (TZC) (35.1% S). Clinical cures in patients with baseline AmpC-overproducing Enterobacterales were 21/26 (81%) in CAZ-AVI group vs 17/20 (85%) in control groups. Against 53 AmpC-overproducing P. aeruginosa isolates, CAZ-AVI (73.6% S) showed greater in vitro activity than AMK (69.8% S), TZC (58.5% S), and MEM (37.7% S). Clinical cures in patients with baseline AmpC-overproducing P. aeruginosa were 12/14 (86%) in CAZ-AVI group vs 9/12 (75%) in control groups. MIC distributions against the same P aeruginosa isolates were CAZ-AVI (MIC50/90, 4/ >64 µg/mL), MVB (MIC50/90, 8/32 µg/mL), and MEM (MIC50/90, 8/32 µg/mL).Table
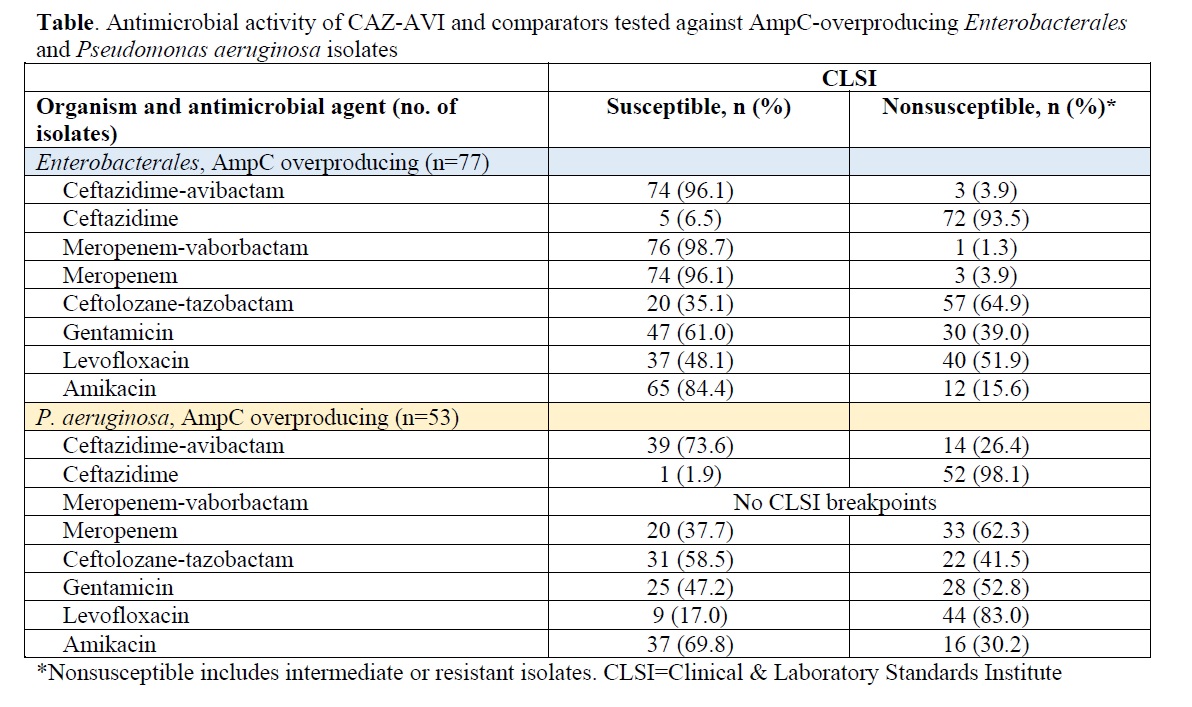
Conclusion: CAZ-AVI was the most active agent against AmpC-overproducing P. aeruginosa with higher proportion of clinical cure than controls. CAZ-AVI was also among the most active agents against AmpC-overproducing Enterobacterales, with >96% isolates susceptible.

