Category: Antimicrobial Stewardship: Program Development and Implementation
Poster Session: Antimicrobial Stewardship: Program Development and Implementation
170 - Development of Key Indicators for Appropriate Antibiotic Use in Republic of Korea: a Systematic Review followed by Delphi Procedure
- BK
Bongyoung Kim
Associate Professor
Department of Internal Medicine, Hanyang University College of Medicine
Seongdong-gu, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- ML
Myung Jin Lee
Assistant professor
Department of Internal Medicine, Inje University Sanggye-Paik Hospital, Seoul, South Korea
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.

Se Yoon Park
Assistant professor
fectious Diseases, Department of Internal Medicine, Soonchunhyang University Seoul Hospital, Seoul, Korea
seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- SM
Song Mi Moon
Associate Professor, Division of Infectious Diseases
Seoul National University College of Medicine
Seoungnam-si, Kyonggi-do, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- KS
Kyung Ho Song
Professor
Seoul National University College of Medicine
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- TK
Tae Hyong Kim
Professor
Division of Infectious Diseases, Department of Internal Medicine, Soonchunhyang University Seoul Hospital
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- EK
Eu Suk Kim
Dr
Seoul National University Bundang Hospital
Bundang-gu, Kyonggi-do, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- HK
Hong Bim Kim
Professor
Seoul National University College of Medicine
Seoul, Seoul-t'ukpyolsi, Republic of KoreaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
Co-Author(s)
Presenting Author(s)
Co-Author(s)
Background:
The aim of this study was to develop a set of key quality indicators (QIs) for application to nationwide point surveillance of appropriateness of antibiotic usage in Republic of Korea.
Methods:
A systematic literature review was performed in order to retrieve a list of potential key QIs. These candidates were evaluated by multidisciplinary expert panel using a RAND-modified Delphi procedure, using two online questionnaires and a face-to-face meeting between them. Twenty-five expert panels with diverse backgrounds (infectious diseases specialist, urologist, laboratory medicine doctors, pediatric infectious disease specialists, otorhinolaryngology doctors, gastrointestinal doctors, pulmonologist, general surgeon, and researcher in National Evidence-Based Healthcare Collaborating Agency) participated in the consensus procedure. A Likert scale (ranging 1-7) was used for the evaluation of appropriateness of the potential key QIs and items with median score 6 or 7 were accepted if there was no disagreement. In addition, we grade each QI into admission, outward, or surgical prophylaxis using the Likert scale. If the score was 6 or 7, we considered it as appropriate application.
Results: The systematic literature review identified 23 potential QIs, from 21 studies. Ultimately, 17 key indicators were retained, with a high level of agreement (13 QIs for admitted patients, 7 for outward patients and 3 for surgical prophylaxis) (Figue 1). After sum of importance score and applicability, 6 key QIs [6 QIs (1-6) for admitted patients and 3 (1, 2 and 5) for outward patients] were finally selected: (1) prescribe empirical antibiotic therapy according to guideline, (2) change empirical to pathogen-directed therapy, (3) take cultures from suspected sites of infection, (4) take 2 blood cultures, (5) adapt antibiotic dosage to renal function, and (6) document antibiotic plan (Table 1). In surgical prophylaxis, prescribe according to guideline and initiate antibiotics one hour before incision was finally selected (Table 2).Figure 1. Flowchart of the study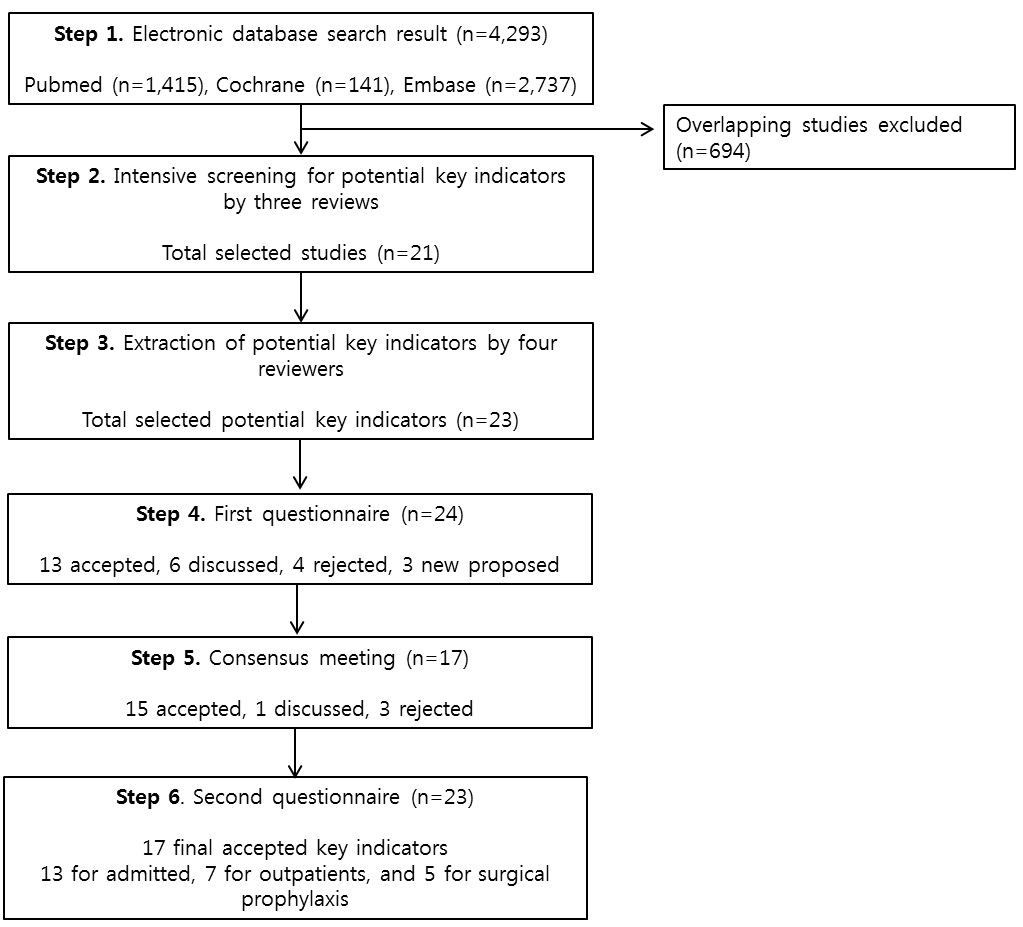 Table 1. Ranking in key indicators for admitted and out patients and applicability in point surveillance study.
Table 1. Ranking in key indicators for admitted and out patients and applicability in point surveillance study.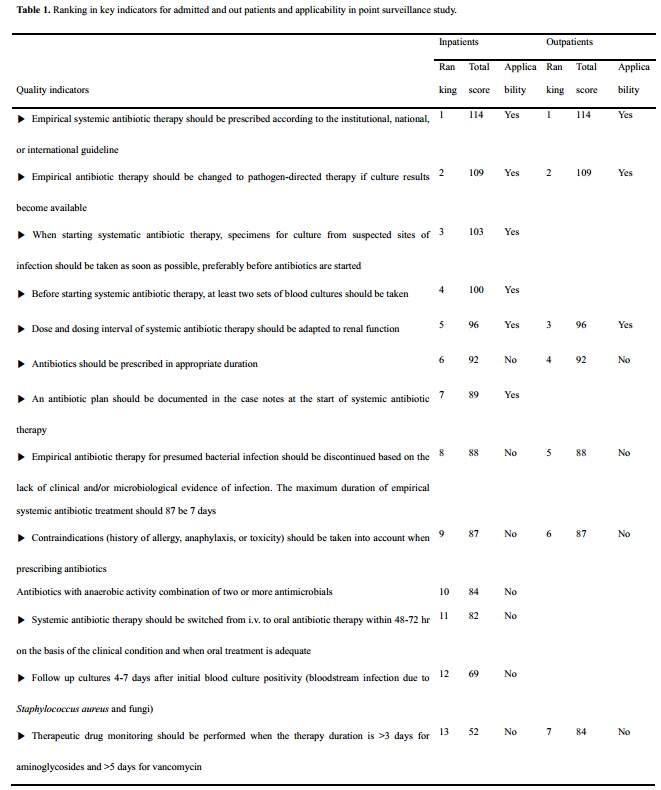 Table 2. Ranking in key indicators for surgical prophylaxis and applicability in point surveillance study.
Table 2. Ranking in key indicators for surgical prophylaxis and applicability in point surveillance study.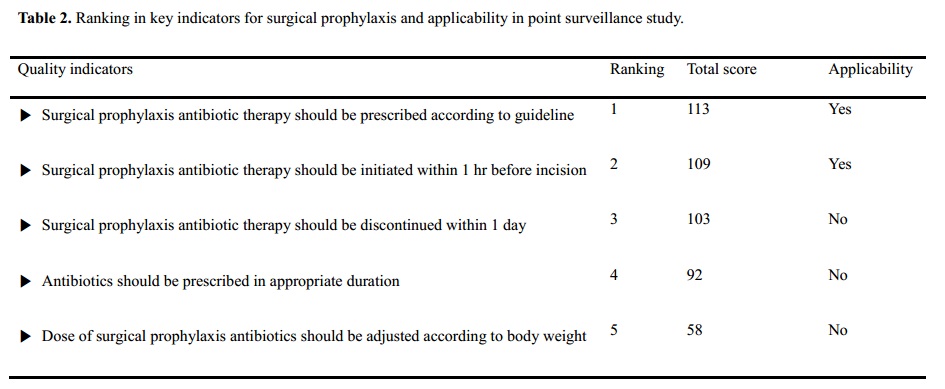
Conclusion: We identified key QIs to measure the appropriateness of antibiotics. These QIs can be used to identify targets for improvement and to evaluate the effects of antibiotic stewardship intervention.

