Category: HIV: Epidemiology and Screening
Poster Session: HIV: Epidemiology and Screening
968 - The Impact of Opt-Out HIV Screening and Patient Navigator-Assisted Linkage to Care of Newly Diagnosed Persons with HIV in a High-Prevalence Emergency Department

Swetha Kodali
Medical Student
Rutgers New Jersey Medical School
Newark, New JerseyDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.

Jeffrey M. Paer
Medical Student (MS4)
Rutgers New Jersey Medical School, Newark, NJ
Bloomfield, New JerseyDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.

Alexander W. Sudyn
Medical Student
Rutgers New Jersey Medical School
Newark, New JerseyDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- SM
Samuel Maldonado
Resident Physician
University of Virginia
Charlottesville, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- AN
Amesika Nyaku
Assistant Professor
Rutgers New Jersey Medical School
Newark, New JerseyDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- SS
Shobha Swaminathan
Associate Professor
Rutgers New Jersey Medical School
Newark, New JerseyDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
Presenting Author(s)
Co-Author(s)
Background:
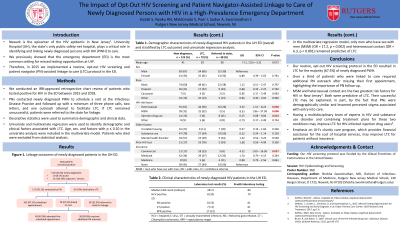
Newark is the epicenter of the HIV epidemic in New Jersey. University Hospital, the state’s only public safety net hospital, plays a critical role in identifying and linking newly diagnosed persons with HIV (PWH) to care. We previously showed that the emergency department (ED) is the most common setting for missed testing opportunities. Therefore, in 2015 we implemented a routine opt-out HIV screening and patient navigator (PN)-assisted linkage to care (LTC) protocol in the ED, and this project examined the LTC rates for newly diagnosed PWH.
Methods:
We conducted an IRB-approved retrospective chart review of patients who tested positive for HIV in the ED between 2015 and 2018. Descriptive statistics were used to summarize demographic and clinical data. Univariate and multivariate regression were used to identify demographic and clinical factors associated with LTC for newly diagnosed PWH. Age, sex, and factors with p ≤ 0.10 in the univariate analysis were included in the final model.
Results:
Of the 464 patients who screened positive, 123 (26.5%) were new diagnoses. The mean age was 41.0 years (SD = 13.8); 82 (67%) male; 74 (60%) black, 26 (21%) Hispanic, 7 (6%) white. The median CD4 count was 242 (IQR = 120 - 478) cells/µL, and 10 patients (8.1%) had acute HIV infection. Six patients (4.9%) died before LTC. Among the remaining 117 patients, PN outreach resulted in scheduled appointments at the Infectious Disease Practice for 102 (87.2%). In total, 79 (67.5%) were linked to care and 38 (32.5%) were referred to the state for linkage. Of the patients linked to care, 49 (62.0%) attended their first appointment and 30 (38.0%) required additional PN outreach. Men who have sex with men (MSM) (OR = 17.2, p = 0.002) and heterosexual contact (OR = 6.3, p < 0.001) were predictive of LTC.
Conclusion:
Our protocol resulted in LTC for the majority of newly diagnosed PWH. Among those linked to care, over a third required additional PN outreach after missing their first appointment, highlighting the importance of PN follow-up. MSM and heterosexual contact, the two highest risk factors for HIV in New Jersey, were predictive of LTC. Their successful LTC may be explained, in part, by the fact that PNs were demographically similar and lessened perceived stigma associated with entry into care.

