Category: Bacteremia
Poster Session: Bacteremia
298 - Multicenter retrospective cohort study of the clinical significance of Staphylococcus lugdunensis isolated from a single blood culture set

Naomi Hauser
Infectious Diseases fellow
University of Maryland Medical Center, CaliforniaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JK
Justin Kim
Infectious Disease Fellow
University of Maryland Medical Center
Baltmore, MarylandDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- PL
Paul Luethy
Dr
University of Maryland School of Medicine
Baltimore, MDDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- SS
Sarah Schmalzle
Assistant Professor of Medicine
University of Maryland School of Medicine
Baltimore, MarylandDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.

JACQUELINE T. BORK
Assistant Proferssor
University of Maryland School of Medicine
Severna Park, MarylandDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
Presenting Author(s)
Co-Author(s)
Background:
Staphylococcus lugdunensis is a coagulase negative Staphylococcus (CoNS) species with the potential to cause aggressive infection. Guidance surrounding S. lugdunensis bacteremia (SLB) is lacking, especially in the case of a single positive set of blood cultures.
Methods:
We performed a multicenter, retrospective observational cohort review of adult patients with SLB from at least one blood culture set within the University of Maryland Medical System from November 2015-November 2019. Objectives were to (1) describe baseline characteristics, (2) compare available criteria for evaluating clinical significance, and (3) evaluate the clinical outcomes among patients with SLB in 1 vs ≥2 positive blood culture sets. Descriptive statistics with Chi-squared and Mann-Whitney U tests were carried out.
Results:
There were 5,548 CoNS-positive blood culture sets, 49 (0.88%) with S. lugdunensis comprising 36 adult patients (24 with 1 positive set and 12 with ≥2 positive sets). Patients with ≥2 positive sets were more likely to be on hemodialysis (HD) (p=0.029) and to have an HD catheter present (p=0.10) (Table 1). Thirty-five of the 36 patients fulfilled at least one of the following: systemic inflammatory response syndrome (SIRS), Souvenir criteria, or clinical criteria (infectious focus on imaging and/or second positive culture site) (Table 2). Twenty-eight (78%) patients were treated with antimicrobial therapy and/or central line removal. SIRS criteria were met more often among patients with 1 positive set (p=0.05). Patients with ≥2 positive sets were more often treated with antibiotics for longer than 2 weeks (p=0.02). The mean time of positive cultures to discharge was 11 days and was longer for patients with only one set of positive blood cultures (13 vs. 6 days), although this difference was not statistically significant (p=0.29) (Table 3).
Table 1. Baseline characteristics
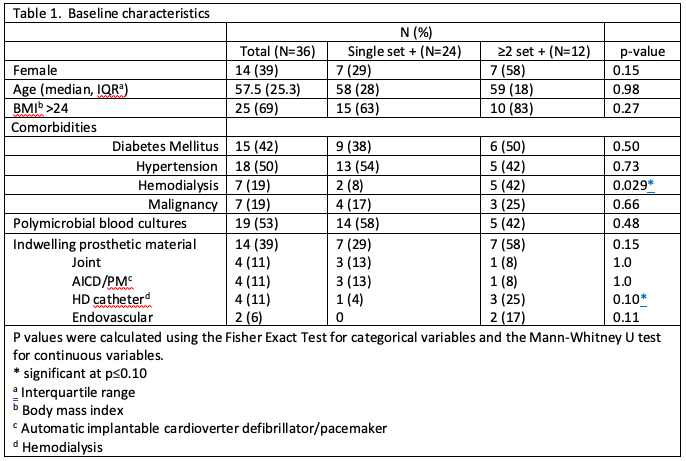 Table 2. Clinically significant S. lugdunensis bacteremia by criteria
Table 2. Clinically significant S. lugdunensis bacteremia by criteria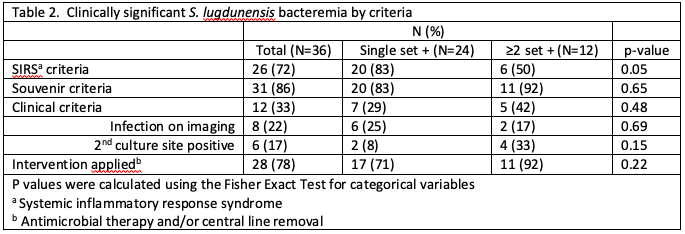 Table 3. Outcomes of those with treated S. lugdunensis in blood cultures
Table 3. Outcomes of those with treated S. lugdunensis in blood cultures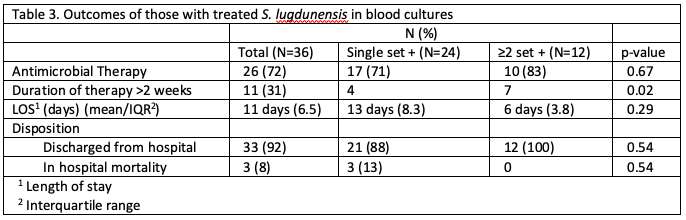
Conclusion:
SLB was rare and occurred more frequently as a single set of positive blood cultures. Though limited by sample size, this study found similar patient characteristics, clinical significance and outcomes between patients with one set and those with ≥2 sets of blood cultures positive for S. lugdunensis. Given the potential severity of SLB, it seems prudent to treat S. lugdunensis in a single blood culture, but larger studies are needed.

