Category: Antimicrobial Stewardship: Program Development and Implementation
Poster Session: Antimicrobial Stewardship: Program Development and Implementation
174 - Impact of Cascade Reporting of Antimicrobial Susceptibility on Antimicrobial Consumption at a Veterans Affairs Medical Center

Nicole C. Vissichelli
Assistant Professor
Virginia Commonwealth University Health System
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- CO
Christine M. Orndahl
Ms.
Virginia Commonwealth University
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JC
Jane A. Cecil
Chief, Infectious Diseases
Central Virginia VA Health Care System
Glen Allen, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- EH
Emily Hill
Director, Clinical Microbiology Laboratory
Central Virginia VA Health Care System
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- RS
Roy T. Sabo
Associate Professor
Virginia Commonwealth University
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- MS
Michael Stevens
Associate Professor
Virginia Commonwealth University Health System
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- DT
Daniel Tassone
Daniel Tassone, PharmD, BCPS
Central Virginia VA Health Care System
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- LV
Leroy Vaughan
Staff Physician in Infectious Diseases, Hospital Epidemiologist
Central Virginia VA Health Care System
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JM
John D. Markley
Infectious Diseases Physician
Richmond VA Medical Center, VCU Medical Center
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- MH
Matthew M. Hitchcock
Staff Physician in Infectious Diseases
Central Virginia VA Health Care System
Midlothian, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
Presenting Author(s)
Co-Author(s)
Background:
Cascade reporting (CR) is a strategy of reporting antimicrobial susceptibility test results in which secondary agents are only reported if an organism is resistant to primary, narrow spectrum agents within a drug class. A multidisciplinary team developed CR algorithms for Gram-negative bacteria based on the local antibiogram and infectious diseases practice guidelines.
Methods:
CR was implemented at a 399-bed tertiary care VAMC in March 2018. In a quasi-experimental study, antimicrobial use data across 8 inpatient units were extracted from the CDC’s NHSN AU module from April 2017 – March 2019 (12 months pre- and post-implementation of CR), reported as antimicrobial days of therapy (DOT) per 1000 days present (DP). T-tests and linear mixed models accounting for seasonal and random unit effects were used to compare antimicrobial use pre- and post-CR implementation.Figure 1A. Cascade reporting algorithm for antimicrobial susceptibility reporting for Enterobacteriaceae.jpg) Figure 1B. Cascade reporting algorithm for antimicrobial susceptibility reporting for Pseudomonas aeruginosa
Figure 1B. Cascade reporting algorithm for antimicrobial susceptibility reporting for Pseudomonas aeruginosa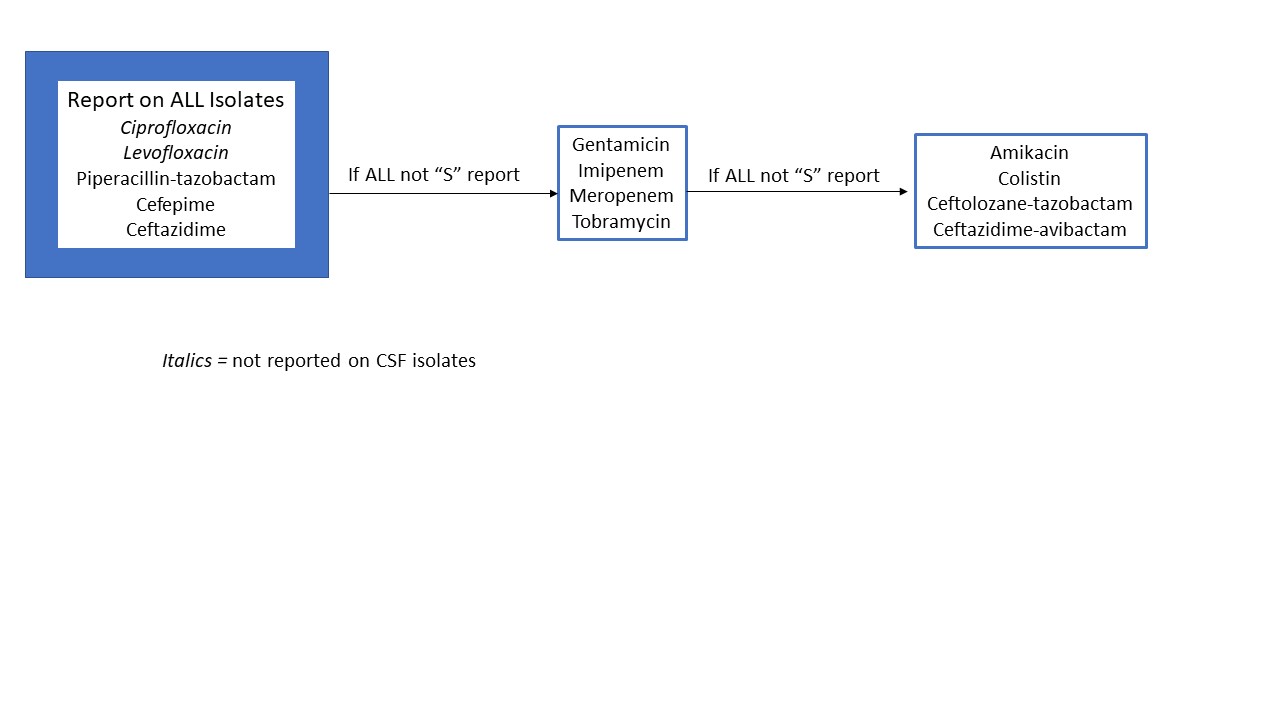
Results:
Following CR implementation, mean monthly meropenem (p=0.005) and piperacillin/tazobactam (p=0.002) use decreased, while cefepime use increased (p< 0.001). The slope of ciprofloxacin use decreased by 2.16 DOTs/1,000 DP per month (SE=0.25, p< 0.001). The slope of cefpodoxime and moxifloxacin use decreased by 18% (p< 0.001), and 7% (p< 0.001), respectively. The slope of cephalexin use decreased by 0.55 DOTs/1,000 DP (SE=0.26, p< 0.001). The slope of ceftriaxone and cefepime use increased by 1.51 (SE=0.59, p=0.011) and 1.06 (SE=.32, p=0.002) DOTs/1000 DP per month, respectively. There were no significant changes in the slope of amoxicillin/clavulanate, levofloxacin, or meropenem consumption. Rates of Clostridioides difficile infection did not significantly change.Figure 2A. Average monthly use of oral antibiotics across all units in average days of therapy (DOTs) per 1000 days present. CR = Cascade reporting. *For Cefpodoxime and moxifloxacin medians were reported as data was not normally distributed.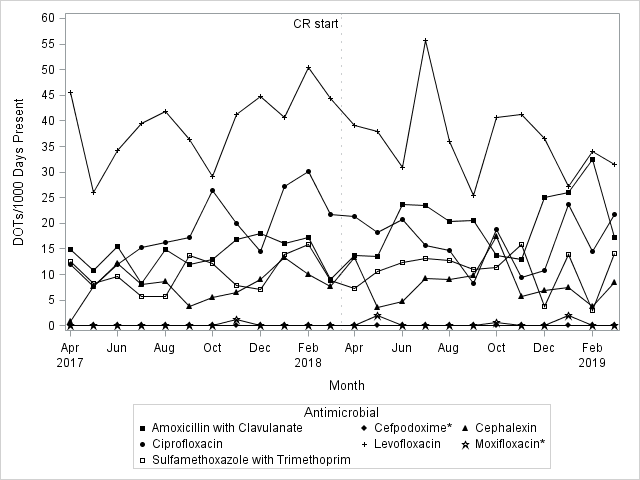 Figure 2B. Average monthly use of intravenous antibiotics across all units in average days of therapy (DOTs) per 1000 days present. CR = Cascade reporting.
Figure 2B. Average monthly use of intravenous antibiotics across all units in average days of therapy (DOTs) per 1000 days present. CR = Cascade reporting.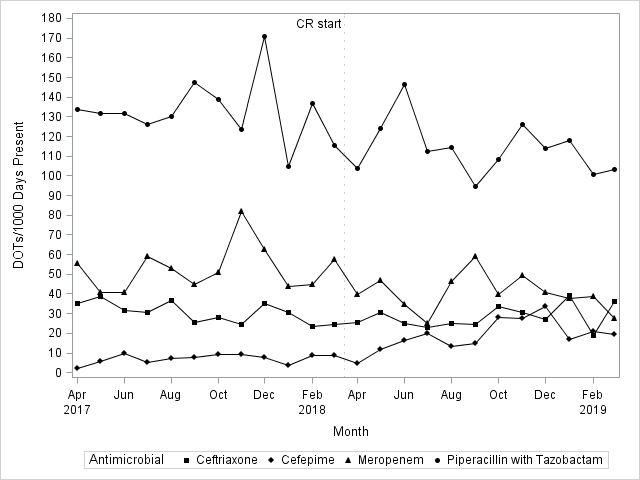 Table 1. Slope of Antimicrobial Utilization Pre and Post-Cascade Reporting Implementation.
Table 1. Slope of Antimicrobial Utilization Pre and Post-Cascade Reporting Implementation.
Conclusion:
After implementation of CR, the slope of ciprofloxacin use decreased and mean monthly meropenem use decreased. CR is a valuable tool that can be employed by ASPs to encourage optimal use of antibiotics.

