Category: HIV: Complications and Special Populations
Poster Session: HIV: Complications and Special Populations
927 - Antiretroviral Laboratory Monitoring and Implications for HIV Clinical Care in the Era of COVID-19 and Beyond
- LF
Lori E. Fantry
Professor of Medicine
University of Arizona
TUCSON, ArizonaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.

Lawrence York
Dr.
University of Arizona
TUCSON, ArizonaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- Jf
Julia fisher
Dr.
University of Arizona Health Science
Tucson, ArizonaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- ja
jessica august
Dr.
santa rosa kaiser hospital
Santa Rosa, CaliforniaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- jm
jose marquez
Dr.
University of Arizona
tucson, ArizonaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- KE
Kristen Ellis
Dr.
University of Arizona Health Science Center
tucson, ArizonaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- LM
Lakshmi Malladi
Ms.
University of Arizona
tucson, ArizonaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- AK
Ashwini Kaveti
Ms.
University of Arizona
tucson, ArizonaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- MK
Marine Khachatryan
Ms.
University of Arizona
Tucson, ArizonaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- Mp
Marissa paz
Ms.
University of Arizona
tucson, ArizonaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- MA
Matthew Adams
Dr.
University of Arizona
tucson, ArizonaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- eB
edward Bedrick
Dr.
University of Arizona Health Science Center
tucson, ArizonaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
Co-Author(s)
Presenting Author(s)
Co-Author(s)
Background:
In the era of COVID-19, providers are delaying laboratory testing in people with HIV (PWH) to avoid unnecessary exposures despite antiretroviral guidelines recommending periodic testing. The purpose of this study was to examine the clinical significance of periodic renal, liver, and lipid testing. Characteristics of Participants at the Initial Visit (N-261).png) Percentage of Indiviudals with GFR ≥ 60 ml/min
Percentage of Indiviudals with GFR ≥ 60 ml/min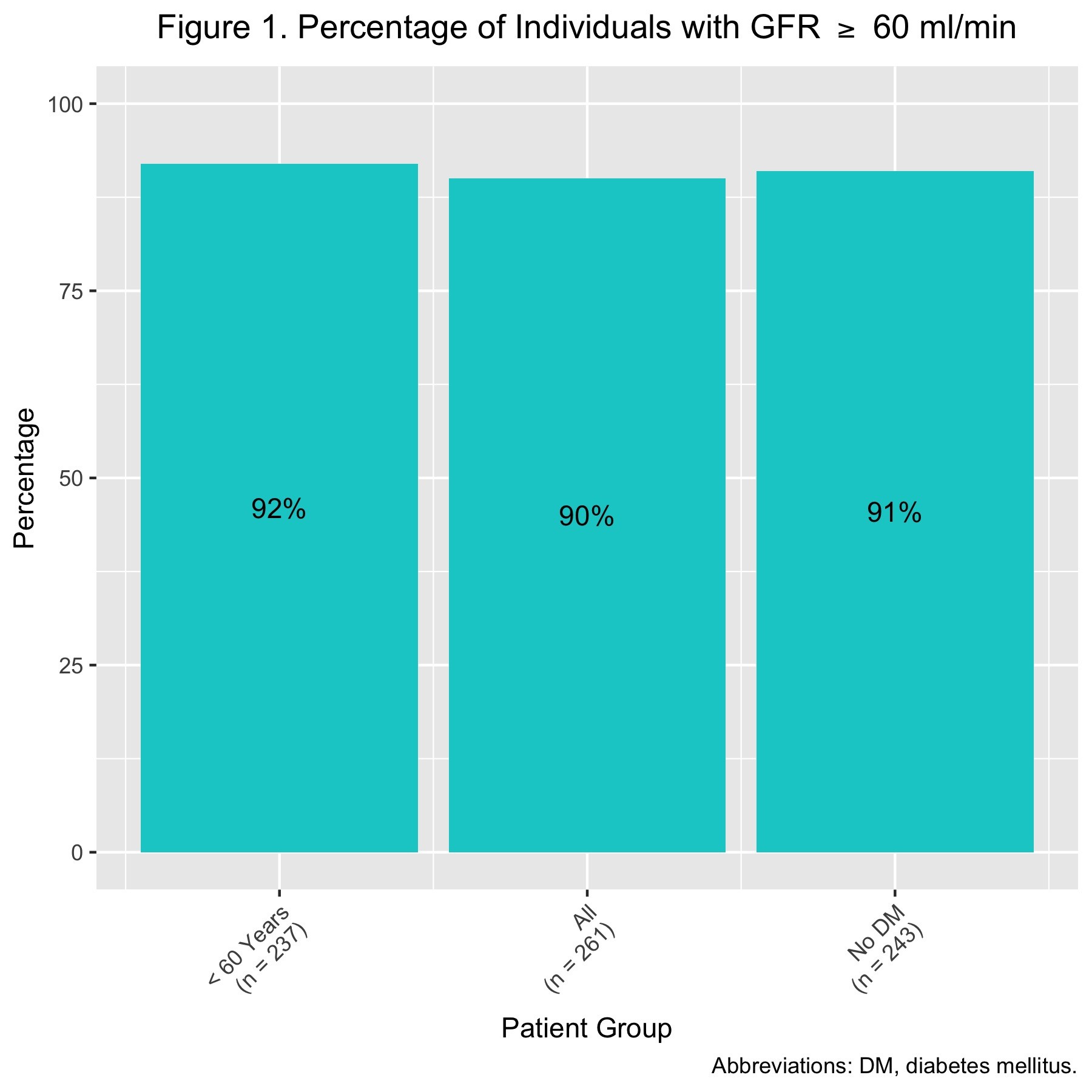
Methods: We reviewed the charts of 265 people with HIV (PWH) who initiated outpatient care at HIV clinic between 1/1/16 and 12/21/18 and had at least two clinic visits. Analysis included frequency distributions, descriptive statistics, one-sided binomial exact tests, and Poisson models with 95% confidence intervals (CI).Actions Taken in Response to GFR < 60 or ALT or AST > 2X ULN.png) Actions Taken Following Lipid Labs
Actions Taken Following Lipid Labs
Results:
Eighty-five percent (221) of PWH had no laboratory abnormalities while on antiretroviral therapy (ART). The most common abnormality was a glomerular filtration rate (GFR) < 60 ml/min found in 10% of PWH. Multivariate analysis revealed that diabetes mellitus (DM) was associated with an increased risk of GFR < 60 ml/min (estimated rate ratio 2.68, 95% CI 1.35-5.33) and age < 60 years (estimated rate ratio .122, 95% CI .05-.32) was associated with a decreased risk (estimated rate ratio .24, CI .14 –.43). When a GFR was < 60 ml/min or an AST or ALT was >2X upper limit of normal (ULN), no action was taken in 52% of the cases. When an action was taken, the most
common action was to repeat testing (18%). After a lipid panel result, the most common actions were to calculate a 10-year cardiovascular risk score (32%) and add a statin (18%). Taking action after lipid panel results was strongly associated with age ≥ 40 (estimated rate ratio 9.1, 95% CI 3.3-25). ART was changed in seven PWH based on GFR, AST/ALT, or lipid panel results. There were four individuals with poor outcomes including cerebrovascular accident, acute renal failure, end stage renal disease, congestive heart failure, myocardial infarction, and death. Contributing factors were hypertension, DM, and hypercholesterolemia.
Conclusion:
Individuals < 40 years without ithout comorbidities had a low risk of having clinically significant renal and liver function abnormalities and rarely had actions taken after renal, liver, or lipid results. In the era of COVID-19 and beyond, it may be prudent for in certain groups to delay or eliminate liver, renal, and lipid testing to eliminate exposure, reduce cost, and avoid patient anxiety.

