Category: Antimicrobial Stewardship: Outcomes Assessment (clinical and economic)
Poster Session: Antimicrobial Stewardship: Outcomes Assessment (clinical and economic)
74 - Interrupted Time Series Analysis of the Impact of Fluoroquinolone Cascade Reporting

Matthew Nestler
Medical Student
Virginia Commonwealth University School of Medicine
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JM
John D. Markley
Infectious Diseases Physician
Richmond VA Medical Center, VCU Medical Center
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- AN
Andrew Noda
Dr
Virginia Commonwealth University Health System
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- EG
Emily Godbout
Assistant Professor
Virginia Commonwealth University Health System
Richmond, VADisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- JK
Jihye Kim
Clinical Pharmacist, Infectious Diseases/ASP
VCU Health System
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- KL
Kimberly B. Lee
Clinical Pharmacist, Antimicrobial Stewardship
Virginia Commonwealth University Health System
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- CD
Christopher Doern
Director, Clinical Microbiology
Virginia Commonwealth University Health System
Richmond, VADisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- AB
Alexandra L. Bryson
Associate Director of Clinical Microbiology, Assistant Professor of Pathology
Virginia Commonwealth University Health System
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.

Michelle Doll
Associate Professor
Virginia Commonwealth University Health System
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.

Gonzalo Bearman
Professor
Virginia Commonwealth University Health System
Richmond, VADisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- MS
Michael Stevens
Associate Professor
Virginia Commonwealth University Health System
Richmond, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
Presenting Author(s)
Co-Author(s)
Background:
Cascade reporting is a form of selective reporting where antibiotic susceptibility results are revealed in a sequential order to optimize antibiotic use. On May 1, 2019, Virginia Commonwealth University Health implemented cascade reporting for ciprofloxacin and levofloxacin for E. coli from urine cultures. We hypothesize that suppressing fluoroquinolone (FQ) results for urine isolate E. coli susceptibility panels using cascade reporting led to a decrease in the overall rate of inpatient FQ use.
Methods:
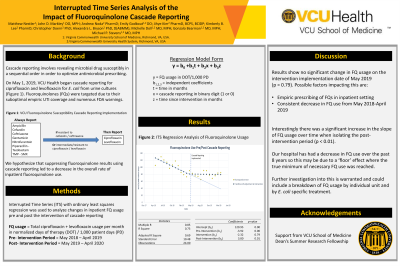
We compared inpatient FQ use (in days of therapy (DOT)/1000 patient days (PD)) for the one-year pre-cascade period (May 2018-April 2019) to the one-year post cascade period (May 2019-April 2020). Inpatient FQ use for May 2018-April 2020 was modeled as an interrupted time series (ITS) using ordinary least squares regression. The regression model followed the form of Y = B0 +B1T + B2 X + B3 XT with Y = (DOT/1,000 PD), T = time in months, X = cascade reporting represented with a binary digit, and XT= time since cascade reporting was implemented. Results were examined for autocorrelation and lag effects. Analysis conducted using Microsoft Excel and Python Statsmodel library v0.11.1.
Results:
A segmented regression model was successfully fitted with R^2 = 0.73 (Figure 1). The pre-intervention slope (T), intervention change (X), and post-intervention slope (XT) were -3.9, -2.3, and 3.8 DOT respectively. A significant positive change in pre versus post intervention slope was detected (p = 0.01).Figure 1: Fluoroquinalone Use Pre/Post Cascade Reporting.png)
Conclusion: Results showed no significant change in FQ DOT/1000 PD when cascade reporting was implemented in May 2019. This may be due to empiric prescribing of FQs in the inpatient setting, due to the fact the rate of FQ use was already decreasing prior to cascade reporting adoption, or due to other factors.
We detected a significant positive change in the slope of FQ from -4 to 4 DOT/1000 PD each month post-cascade reporting. Our hospital has had a decrease in FQ use over the past 8 years so this may be due to a ‘floor’ effect where the true minimum of necessary FQ use was reached; further investigation is warranted. We believe our data will be of interest to other Antimicrobial Stewardship Programs considering cascade reporting.

