Category: Antimicrobial Stewardship: Trends in Antimicrobial Prescribing
Poster Session: Antimicrobial Stewardship: Trends in Antimicrobial Prescribing
244 - The Double-Edged Sword of Cost Effectiveness in Evaluating Antimicrobial Stewardship Interventions

Omar Zmerli
Infectious Diseases Research Fellow
Saint George Hospital University Medical Center - University of Balamand
Beirut, Beyrouth, LebanonDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- AC
Amanda Chamieh
ID Specialist
Saint George Hospital University Medical Center
Beirut, Beyrouth, LebanonDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- SS
Sanaa Saliba
ID Fellow
Saint George Hospital University Medical Center
Beirut, Beyrouth, LebanonDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- CA
Claude Afif
ID Specialist
Saint George Hospital University Medical Center
Beirut, Beyrouth, LebanonDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- EA
Eid Azar
ID Specialist
Saint George Hospital University Medical Center
Beirut, Beyrouth, LebanonDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
Presenting Author(s)
Co-Author(s)
Background:
The multiple classical benefits of reducing antimicrobial consumption extend beyond the impact on rates of antimicrobial resistance and infections to include a cost-saving effect of 100,000$-300,000$ per intervention as estimated by the CDC. However, the recent introduction of novel antimicrobial molecules with a high price tag and the fall in the prices of older agents presents a substantial challenge in maintaining cost-effectiveness.
Methods:
We retrieved from the antimicrobial stewardship program(ASP) database the consumption of the Gram-negative broad-spectrum antibacterial agents (GNBS): imipenem, meropenem, ertapenem, piperacillin-tazobactam, amikacin, colistin, ceftazidime, ceftolozane-tazobactam and cefepime from January 2015-August 2019 at Saint George Hospital(SGH), a 333-bed tertiary care center in Lebanon. The yearly cost of all antibacterials consumed during this period were obtained from SGH billing records. GNBS consumption was calculated as Daily Defined Doses (DDD)/1000 Patient Days(PD) per WHO guidelines.
Results: The carbapenem consumption significantly dropped from a peak of 205 DDD/1000PD in 2015 to 33 DDD/1000PD in 2019. This drop was not accompanied by an increase in the consumption of other GNBS. The total use of GNBS dropped by 54% from 288 DDD/1000PD in 2015 to 132 DDD/1000PD by August 2019. Currently, SGH serves a yearly average of 82,000 patient-days. Hence, this reduction in total GNBS consumption corresponds to 12,792 fewer daily defined doses of antimicrobial therapy per year.
The average annual cost of all antibacterials at SGH is 1,100,000 $ (U.S. Dollars), ranging from 955679 $ to 1340109 $ for the period 2015-2019. (Table 1)Consumption of Gram-negative Broad-Spectrum Antimicrobial Agents and Cost of Antibiotics at Saint George Hospital, Lebanon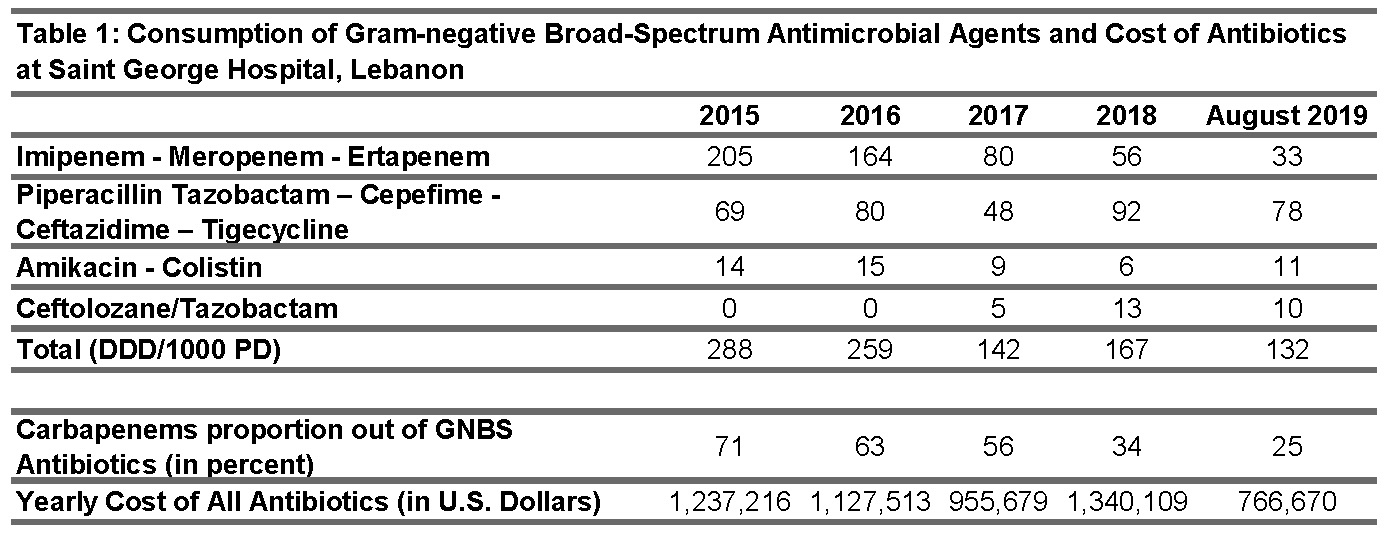
Conclusion:
The striking decrease in GNBS consumption, namely carbapenems, was not mirrored with a reduction of total antibacterial cost. Although novel antimicrobials carry great potential, they come at a significant increase in overall cost. Modeling ASP interventions solely around cost-effectiveness will limit the better placement of these new agents in institutional therapeutic guidelines. Strict continuous analysis of consumption, antimicrobial resistance, and cost within an ASP provides a proactive and vigilant approach to navigate through the complexity of difficult to treat bacterial infections.

