Category: HAI: C. difficile
Poster Session: HAI: C. difficile
789 - Evaluation of Bezlotoxumab for Prevention of Recurrent Clostridioides difficile Infection in Patients at High Risk for Recurrence

Tanner M. Johnson
PGY2 Infectious Diseases Pharmacy Resident
UCHealth University of Colorado Hospital
Denver, ColoradoDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- AH
Amanda Howard
Clinical Pharmacist
UCHealth University of Colorado Hospital
Aurora, ColoradoDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- KS
Kerry Schwarz
Research Pharmacist
University of Colorado Hospital
aurora, CODisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.

Lorna Allen
Infectious Diseases Nurse Practitioner
UCHealth University of Colorado Hospital
Aurora, ColoradoDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.

Misha Huang
Physician, Director of Antimicrobial Stewardship
University of Colorado Anschutz Medical Center
Aurora, CODisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- VB
Valida Bajrovic
Transplant Infectious Diseases Physician
UCHealth University of Colorado Hospital
Aurora, ColoradoDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- mm
matthew miller
university of colorado hospital
parker, CODisclosure: Allergan (Speaker's Bureau)Tetraphase (Speaker's Bureau)
Presenting Author(s)
Co-Author(s)
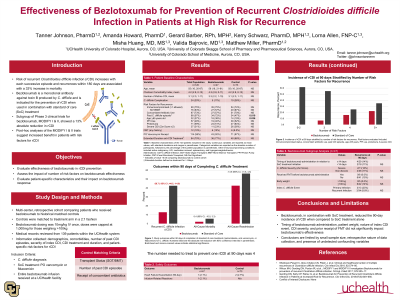
Background: Recurrent Clostridioides difficile infection (rCDI) within 180 days of the index episode is associated with a 33% increase in mortality and, to-date, few treatment options exist to prevent recurrent infection. Bezlotoxumab (BEZ) is a novel therapeutic option for the prevention of rCDI, yet limited data exist regarding its effectiveness in patients at high-risk for recurrence outside of controlled trials. This study aimed to compare BEZ to a historical standard of care (SoC) cohort for the prevention of rCDI in patients at high risk for recurrence.
Methods:
A multi-center retrospective cohort study of patients within an academic health-system with one or more risk factors for rCDI. Patients received SoC with oral vancomycin (VAN) or fidaxomicin (FDX) from January 2015 to December 2017 or BEZ, in addition to oral SoC, from September 2017 to September 2019. The primary outcome was rCDI within 90 days of completion of oral VAN or FDX. Secondary outcomes included all-cause readmission, all-cause mortality, and safety events at 90 days.
Results: One-hundred twenty patients received BEZ in addition to SoC (n=47) or SoC alone (n=73). Mean (SD) age was 55 (16) years, mean (SD) number of lifetime CDI was 3 (2) episodes, and 30.8% of patients had severe CDI. Six (12.8%) patients in the BEZ cohort and thirty-one (42.5%) in the SoC cohort experienced rCDI at 90 days [OR (95% CI) = 0.20 (0.07-0.53), p=< 0.01]. Incidence of all-cause mortality (2.1% vs 5.5%, p=0.67) and all-cause readmission (42.6% vs 56.2%, p=0.20) within 90 days were not statistically different between groups. Patient body weight, timing of BEZ administration, CDI severity, nor prior receipt of fecal microbiota transplantation significantly affected BEZ effectiveness. BEZ was well tolerated with one infusion-related reaction. There were no heart failure exacerbations among BEZ recipients and two exacerbations identified from control group.
Conclusion: In patients with at least one risk factor for rCDI, BEZ in addition to SoC was associated with lower rates of recurrent infection than SoC alone and may be a reasonable adjunct therapy in high risk patient populations.

