Category: Antimicrobial Stewardship: Program Development and Implementation
Poster Session: Antimicrobial Stewardship: Program Development and Implementation
185 - Pilot of a Face-to-Face Model of Stewardship (Handshake Stewardship) in a General Medicine Ward
- KM
Kazumi Morita
Clinical Pharmacy Specialist, Infectious Diseases
Temple University Hospital
Philadelphia, PennsylvaniaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- DM
Daniel Mueller
Assistant Professor, Medicine
Temple University Hospital
Philadelphia, PADisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
Presenting Author(s)
Co-Author(s)
Background:
Handshake stewardship (HS) is an antibiotic stewardship strategy that includes a more in-person approach to prospective audit and feedback (PAF). It has emerged as an effective form of PAF, enhancing trust and collaboration between the antibiotic stewardship team (AST) and the prescribers. However, resources can be a barrier to implementation. We sought to describe our experience of a HS pilot implementation at our institution.
Methods:
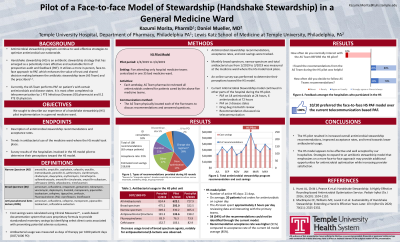
Our HS model was implemented as a pilot among five attending-only hospital medicine teams at Temple University Hospital. All antimicrobials administered to patients on these teams were reviewed by the AST pharmacist on weekdays from 2/4/19 to 3/4/19. The AST physician and pharmacist then physically located each team to discuss recommendations and answered questions. Number and types of AST recommendations were recorded along with the outcome. As patients on all five teams were centralized in one patient care unit (PCU), antibiotic utilization of this PCU, measured as days of therapy per 1000 patient days (DOT/1000 PD) was collected from January to March 2019. An anonymous survey of hospitalists involved in this pilot was also performed to determine their perceptions toward the HS model.
Results:
During the pilot period, 108 recommendations were made on 63 unique patients. On average, 20 patients were on antimicrobials on a given day, and AST spent 2 hours per day reviewing data and interacting with the teams. The most common recommendation was a change in antibiotic regimen (39%), mostly for de-escalation of therapy, with an overall acceptance rate of 91%. Overall antibiotic usage was numerically lower in the pilot month (February; 622 DOT/1000 PD) compared to the two adjacent non-pilot months; January (824 DOT/1000 PD) and March (728 DOT/1000 PD). The difference was mostly explained by the decrease in anti-pseudomonal beta-lactam use. The HS model was widely accepted among the surveyed hospitalists, who preferred it over the current PAF model completed via telecommunication.
Conclusion:
The HS model appears to be effective and well accepted by our hospitalists. Strategies to expand this face-to-face approach may provide additional opportunities for antimicrobial optimization while increasing provider satisfaction.

